|
|
International Journal of Arrhythmia 2012;13(3): 28-34.
|

Introduction
The term “trifascicular block”is confusing
because the involvement of the right bundle branch
and both fascicles of the left bundle branch would
generally manifest as a complete heart block.
Moreover, the term trifascicular block is often
inaccurately applied for cases with a bifascicular
block and prolonged PR interval. Progressive
familial heart block (PFHB) type I is an autosomal
dominant cardiac conduction disorder that may
progress to a complete atrioventricular (AV) block.
Type I PFHB is characterized by a right bundle
branch block (RBBB), left anterior fascicular block
(LAFB), prolonged PR interval, or complete AV
block with broad QRS complexes.1,2

Case
A 29-year-old man presented to our hospital
with a complaint of dizziness. He had experienced 2
episodes of syncope 7 and 25 years ago. Examination
of his family history indicated that his mother had
undergone permanent pacemaker implantation at
the age of 51 years (Figure 1). In addition, 2 of his
uncles had also undergone permanent pacemaker
implantation. On examination, the patient's blood
pressure was 120/80 mmHg, heart rate was 49 bpm,
respiratory rate was 20 times per minute, and body temperature was 36.8℃. An initial electrocardiography
(ECG) indicated atrial flutter with variable
ventricular response and a bifascicular block (RBBB
and LAFB, Figure 2). On echocardiography, a mild
left ventricular systolic dysfunction (ejection
fraction = 50%) with enlargement of both atria was
observed. At admission, he exhibited a seizure-like
motion with syncope, and showed a ventricular
pause up to 16 seconds on 24-hour Holter
monitoring (Figure 3, 4). Subsequently, a temporary
pacemaker was inserted. Radiofrequency catheter
ablation (RFCA) with bidirectional cavotricuspid
isthmus block was then performed for atrial flutter.
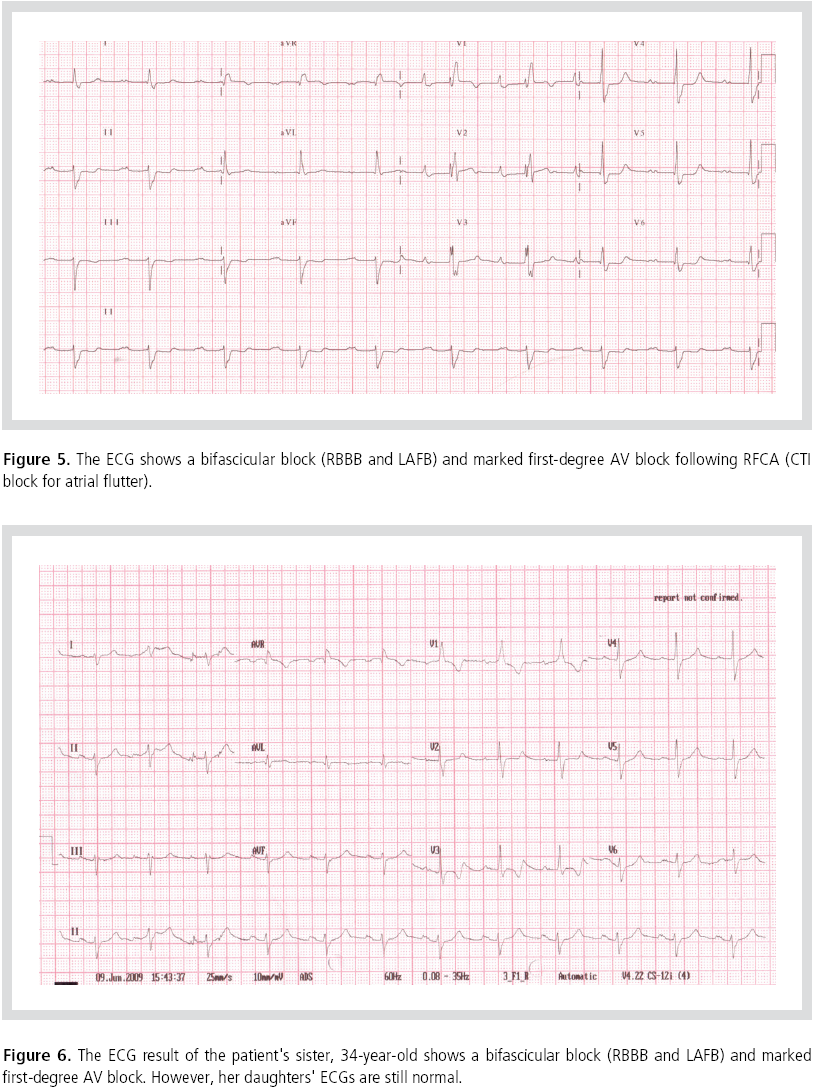
Following RFCA, an additional ECG revealed a bifascicular block (RBBB and LAFB) and marked
first-degree AV block (Figure 5), and 24-hour
Holter monitoring indicated an intermittent
second-degree AV block. Following frequent
episodes of symptomatic high-degree AV block, he
underwent permanent pacemaker implantation
(DDD type). The ECG results of the patient's brother
and sister also indicated a trifascicular block
(Figure 6, 7). However, the ECG results of his
sister's daughters were normal. A few months later,
his brother underwent permanent pacemaker
implantation for complete AV block at another
hospital. The patient's family pedigree showed an
autosomal dominant inheritance (Figure 8).


Discussion
In 1968, Rosenbaum and his colleagues described
the trifascicular nature of the intraventricular
conduction system and the trifascicular block and hemiblock.3 The term “trifascicular block”is confusing,
as the involvement of the 3 fascicles in the ventricle
would generally manifest as a complete heart block.
Therefore, the trifascicular block is often inaccurately
applied to cases with alternating RBBB and LBBB
or prolonged PR interval and bifascicular block.
In 1977, Brink and Torrington described a new
autosomal dominant familial heart disease
(progressive familial heart block), which primarily
affects the conduction tissue of the heart.1,2 The
ECG features of type I PFHB are defined by the
evidence of RBBB, LAFB, prolonged PR interval, or
complete heart block with broad QRS complexes.2
These ECG features can help differentiate type I
PFHB from progressive familial heart block type II
(type II PFHB), wherein the onset of complete heart
block is associated with narrow QRS complexes.2
Type I PFHB manifests symptomatically when
complete heart block develops, and dyspnea,
syncopal episodes, or sudden death are noted. Prompt implantation of a permanent pacemaker is
vital for the successful management of patients with type I PFHB. The use of a prophylactic
pacemaker in these conditions is controversial.4

Follow-up visits and ECGs at 6-month intervals, at
least, are recommended for patients with any degree of heart block, and an annual examination is
recommended for the patient's family members
with normal ECGs.5 Although the global incidence
of type I PFHB is not known, this disease may not
only be confined to South Africa. A few reports
have indicated a familial tendency of bradyarrhythmia
in the Asian population as well.6
References
- Brink AJ, Torrington M. Progressive familial heart block-two
types.
S Afr med J.
1977;52:53-59.
- Van der Merwe P-L, Weymar HW, Torrinton M, Brink AJ.
Progressive familial heart block, part II: clinical and ECG
confirmation of progression-report on 4 cases.
S Afr med J.
1986;70:356-357.
- Rosenbaum MB, Elizari MV, Lazzari JO. The Hemiblocks.
Oldsmar, Florida:Tampa Tracings; 1970.
- Brink PA, Moolman JC, Ferreira, A, Dejager T, Weymar HW,
Martell RW, Torrington M, Vandermerwe PL, Corfield, VA.
Genetic linkage studies of progressive familial heart block, a
cardiac conduction disorder.
S Afr med J.
1994;90:236-240.
- Van der Merwe P-L, Weymar HW, Torrington M, Brink AJ.
Progressive familial heart block (type I): a follow-up study after
10 years.
S Afr med J.
1988;73:275-276.
- Kim WJ, Shim JJ, Kim HS, Lee TH, Jung SM, Lim DS, Hong SK,
Choi RK, Hwang HK. Familial Sick Sinus Syndrome.
Korean Circ J.
2003;33:1155-1160.
|
|
|
|