|
|
International Journal of Arrhythmia 2012;13(4): 25-28.
|
Case
A 54-year-old woman visited an outpatient clinic because of recurrent palpitation. She did
not have a history of any relevant medical illness.
A 12-lead electrocardiogram obtained at the time
of the event demonstrated atrial fibrillation with
rapid ventricular response (Figure 1). The patient
did not complain of palpitation at the clinic and the ECG showed normal sinus rhythm. Typical findings
of hypertrophic cardiomyopathy were found on
performing two-dimensional echocardiography for
the evaluation of structural heart disease (Figure 2).
Amiodarone was prescribed for maintaining sinus
rhythm and we administered a beta-blocker for the
management of hypertrophic cardiomyopathy. The
patient had a low CHADS2 score (0 points) and
CHA2DS2-VASc score (1 point for female gender);
therefore, to prevent cerebral infarction, aspirin
therapy was started.
The palpitations markedly reduced after medication and there were no clinical events during follow up.
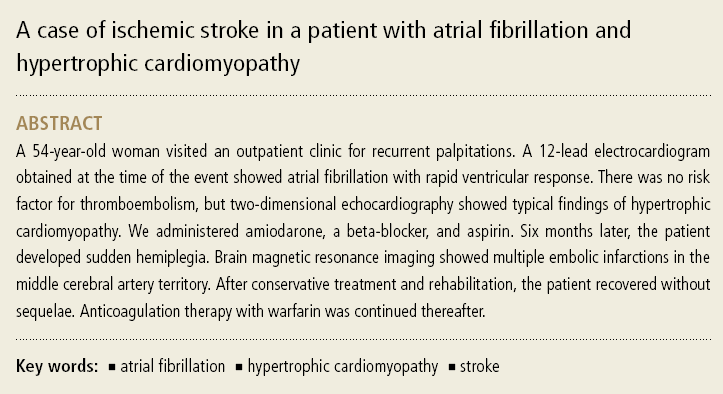
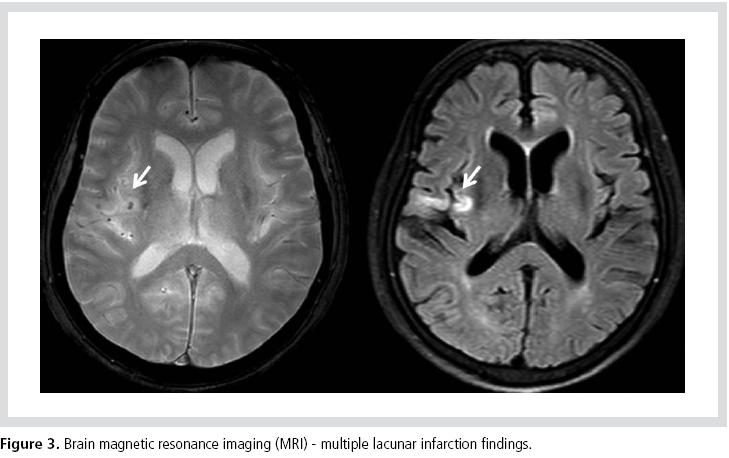
Six months later, however, the patient was admitted to the ER for sudden onset
hemiplegia. Brain MRI showed multiple embolic
infarctions in the temporal and parietal lobes, which
are supplied by the middle cerebral artery (Figure 3).
Consequently, the patient received anticoagulant therapy and rehabilitation treatment. She was then
discharged from hospital without neurologic
sequelae. To prevent recurrent cerebral ischemia,
the patient continued with warfarin therapy as an
outpatient.

Discussion
Cerebral infarction caused by thromboembolism is the principal clinical problem in patients with
atrial fibrillation. Guidelines for anticoagulation therapy should be applied not only to cases of
persistent atrial fibrillation, but also to cases of paroxysmal atrial fibrillation. Various risk factors
have been proposed for the stratification of embolic risk and the CHADS2 scoring system has been
widely used to date. The CHADS2 scoring system is
based on a point system, which includes congestive heart failure, hypertension, advanced age, diabetes,
and a history of ischemic stroke (2 point).
Anticoagulation therapy with warfarin is recommended for patients scoring more than 2
points.1,2 A new scoring system was devised by the
European Society of Cardiology in 2010. The new
scoring system, CHA2DS2-VASc, proposed the
addition of risk factors such as female gender and vascular disease, in addition to the factors in the
CHADS2 scoring system.3 These scoring systems
are applicable to nonvalvular atrial fibrillation.
Patients with mitral stenosis and prosthetic heart valves should undergo anticoagulation with
warfarin, irrespective of scoring.
The CHADS2 score of the patient in this case was 0 and the CHA2DS2-VASc score was 1. Aspirin was
therefore considered sufficient for the prevention of ischemic stroke. However, the initial evaluation
showed typical findings of hypertrophic cardiomyopathy in this patient. In previous studies,
a higher incidence of atrial fibrillation was observed in patients with hypertrophic cardiomyopathy than
in the normal population4 and patients with atrial fibrillation accompanied by hypertrophic
cardiomyopathy had poor clinical outcomes and a higher incidence of cerebral infarction.5
ACC/AHC/ESC guidelines also recommended anticoagulation with wafarin in patients with hypertrophic cardiomyopathy who developed atrial
fibrillation. So consideration for the presence of structural heart disease should precede the application of a scoring system in this present case.
References
- Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen
KA, Halperin JL, Le Heuzey JY, Kay GN, Lowe JE, Olsson SB,
Prystowsky EN, Tamargo JL, Wann S, Smith SC Jr, Jacobs AK,
Adams CD, Anderson JL, Antman EM, Halperin JL, Hunt SA,
Nishimura R, Ornato JP, Page RL, Riegel B, Priori SG, Blanc JJ,
Budaj A, Camm AJ, Dean V, Deckers JW, Despres C, Dickstein K,
Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Tamargo
JL, Zamorano JL. ACC/AHA/ESC 2006 guidelines for the
management of patients with atrial fibrillation: executive
summary: a report of the American College of Cardiology/
American Heart Association Task Force on Practice Guidelines
and the EuropeanSociety of Cardiology Committee for Practice
Guidelines and Policy Conferences (Writing Committee to Revise
the 2001 Guidelines for the Management of Patients With Atrial
Fibrillation) [published correction appears in J Am Coll Cardiol.2007;50:562.
J Am Coll Cardiol.
2006;48:854-9062.
- Byrd CL, Wilkoff BL, Love CJ, Sellers TD, Turk KT, Reeves R,
Young R, Crevey B, Kutalek SP, Freedman R, Friedman R,
Trantham J, Watts M, Schutzman J, Oren J, Wilson J, Gold F,
Fearnot NE, Van Zandt HJ. Intravascular extraction of problematic
or infected permanent pacemaker leads: 1994-1996. U.S.
Extraction Database, MED Institute.
JAMA.
2001;285:2864-2870.
- Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW,
Radford MJ. Validation of clinical classification schemes for
predicting stroke: results from the National Registry of Atrial
Fibrillation.
Europace.
2012;14:1385-1413.
- Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S,
Van Gelder IC, Al-Attar N, Hindricks G, Prendergast B,
Heidbuchel H, Alfieri O, Angelini A, Atar D, Colonna P, De
Caterina R, De Sutter J, Goette A, Gorenek B, Heldal M, Hohloser
SH, Kolh P, Le Heuzey JY, Ponikowski P, Rutten FH. Guidelines
for the management of atrial fibrillation: the Task Force for the
Management of Atrial Fibrillation of the European Society of
Cardiology (ESC).
Eur Heart J.
2010;31:2369-2429.
- Kannel WB, Wolf PA, Benjamin EJ, Levy D. Prevalence, incidence,
prognosis, and predisposing conditions for atrial fibrillation:
population-based estimates.
Am J Cardiol.
1998; 82: 2N-9N.
|
|
|