|
|
International Journal of Arrhythmia 2013;14(2): 29-34.
|
Introduction
The miniaturization of ultrasound transducers
that can be advanced and maneuvered through the
vessels and intracardiac chambers has enabled the
development of intracardiac echocardiography
(ICE). Two modalities of ICE are currently available.
One modality involves the use of a mechanical
nonsteerable catheter with a 360°rotating ultrasound
transducer at the tip (Boston Scientific Co.) that
provides circumferential real-time imaging.1 The
other modality involves the use of a steerable
catheter with a phased array transducer and
variable frequency (Acuson, Siemens). This
ultrasound system supports color, pulsed, and
continuous wave Doppler imaging. The safety and
the effectiveness of mapping and ablation of
premature ventricular complex (PVC)/ventricular
tachycardia (VT) may be enhanced by ICE.2,3 In
patients with outflow tract VT, ICE is an excellent
tool to visualize the great arteries and outflow
tracts. Another advantage of ICE is the ability to
visualize the coronary arteries in relation to the
location of the mapping catheter.3,4
Case #1
64-year-old man presented with a frequent
occurrence of monomorphic PVC and nonsustained
VT, which caused palpitations and dyspnea for 6
months after he had undergone coronary artery bypass grafting following myocardial infarction.
Oral administration of amiodarone (200 mg) was
not effective. Surface electrocardiography (ECG)
showed very narrow QRS, positive V1, and a
superior axis (Figure 1).

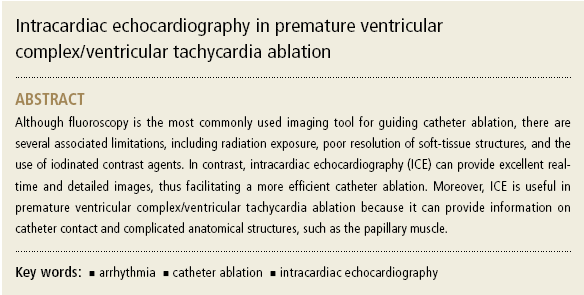
The ablation procedure was performed with the patient in a conscious sedative state. Intracardiac
ECG from the high right atrium, His-bundle site,
coronary sinus, and right ventricular apex region
was simultaneously recorded and displayed using a
surface ECG on a multichannel recorder (Cardiolab,
Prucka Engineering, USA). Voltage mapping
revealed ventricular myocardial scarring in the
inferoseptal wall (Figure 2). The earliest ventricular
activation site during PVC was noted at the border
of the scar at 46 ms before the inscription of
surface QRS waves. ICE clearly showed the location
of the papillary muscle, and papillary muscle origin
PVC was excluded (Figure 3). During ablation, the
PVC morphology was altered. The ablation line was
achieved along the scar border line and no PVC was
observed.
Case #2
A 52-year-old woman presented with frequent
PVC, which had caused dizziness and palpitation
for 1 year (Figure 4). Given the symptomatic and
drug-refractory (β-blocker) nature of the
arrhythmia, radiofrequency (RF) ablation was for this patient. During an electrophysiological
study of the patient under local
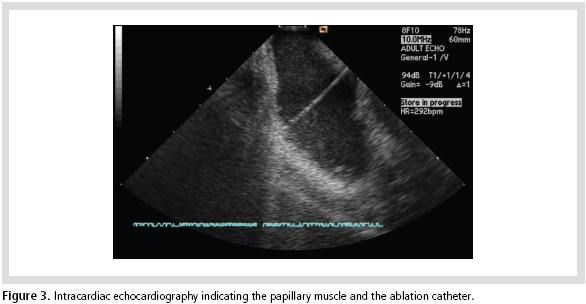
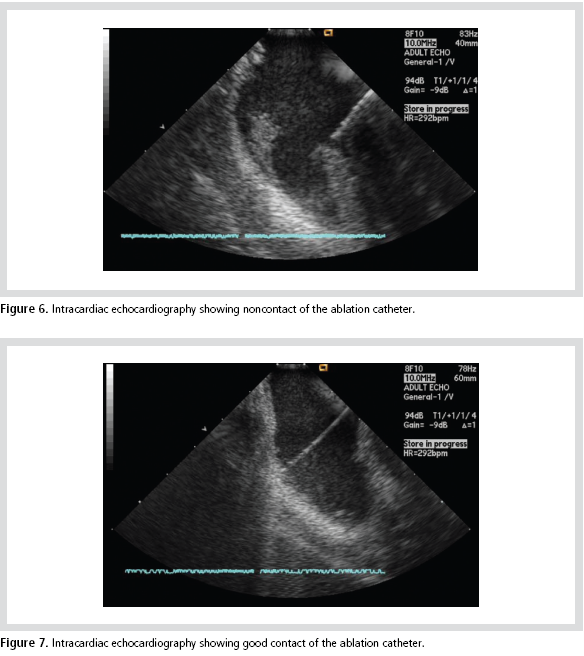
anesthesia, frequent PVCs were observed. The ICE
catheter was inserted into the left femoral vein
through an 8-F introducer sheath and passed into
the right ventricular outflow tract (RVOT). A
clockwise rotational maneuver was performed, and
a short-axis view of the aortic root level was
reached to visualize the RVOT and pulmonic valve
(Figure 5). The ablation catheter did not touch the
cardiac wall (Figure 6), although ECG earlier than
QRS was observed. The earliest ventricular
activation site was noted at 52 ms before the
inscription of surface R-waves, and the ICE
confirmed good contact of the ablation catheter
(Figure 7). Following application of RF energy, the
PVC was not detected. Several additional
radiofrequency catheter ablation procedures were
performed on contiguous lesions circumferentially
surrounding the successfully ablated site. PVC was
not clinically detected after RF ablation during 30
minutes of observation. The patient remained free of symptoms for 3 months.

Discussion
With the constant increase in the number of
individuals experiencing heart failure and the
increased longevity of individuals with coronary
artery disease, ventricular arrhythmias have become
a common clinical problem.5 Catheter ablation can be
offered as an alternative to antiarrhythmic drug therapy as a first-line therapy to patients with
symptomatic ventricular arrhythmias. Ventricular
arrhythmias are associated with complex cardiac
structures, for which the ablation approach depends
on the associated anatomy. The development of ICE
was facilitated by the miniaturization of ultrasound
transducers that are mounted on flexible and
relatively thin catheters, which can be advanced and maneuvered through the vessels and intracardiac
chambers. ICE is an excellent imaging tool to
visualize the great arteries, outflow tracts, and the
coronary arteries in relation to the location of the
mapping catheter. Thus, ICE has led to a significant
improvement in the precision and safety associated
with complex catheter-based ablation procedures.
Decreased radiation exposure, guidance during critical steps in the procedure, visual and real-time
support for precise catheter placement, troubleshooting,
and monitoring of complications are some
of the benefits of real-time continuous ultrasound
imaging.6 Newer technologies, including ICE, have
enabled the development of more accurate and safer
ablation procedures for patients with increasingly
complex arrhythmia substrates.
References
- West JJ, Norton PT, Kramer CM, Moorman JR, Mahapatra S,
DiMarco JP, Mangrum JM, Mounsey JP, Ferguson JD.
Characterization of the mitral isthmus for atrial fibrillation
ablation using intracardiac ultrasound from within the coronary
sinus.
Heart rhythm.
2008;5:19-27.
- Jongbloed MR, Bax JJ, van der Burg AE, Van der Wall EE, Schalij
MJ. Radiofrequency catheter ablation of ventricular tachycardia
guided by intracardiac echocardiography.
Eur J Echocardiogr.
2004;5:34-40.
- Lamberti F, Calo L, Pandozi C, Castro A, Loricchio ML, Boggi A,
Toscano S, Ricci R, Drago F, Santini M. Radiofrequency catheter
ablation of idiopathic left ventricular outflow tract tachycardia:Utility of intracardiac echocardiography.
J Cardiovasc
Electrophysiol.
2001;12:529-535.
- Vaseghi M, Cesario DA, Mahajan A, Wiener I, Boyle NG, Fishbein
MC, Horowitz BN, Shivkumar K. Catheter ablation of right
ventricular outflow tract tachycardia: Value of defining coronary
anatomy.
J Cardiovasc Electrophysiol.
2006;17:632-637.
- Reddy VY, Reynolds MR, Neuzil P, Richardson AW, Taborsky M,
Jongnarangsin K, Kralovec S, Sediva L, Ruskin JN, Josephson ME.
Prophylactic catheter ablation for the prevention of defibrillator
therapy.
N Engl J Med.
2007;357(26):2657-2665.
- Kim, S. S., Hijazi, Z. M., Lang, R. M., & Knight, B. P. The use of
intracardiac echocardiography and other intracardiac imaging
tools to guide noncoronary cardiac interventions.
J Am Coll
Cardiol.
2009;53(23):2117-2128.
|
|
|