|

Introduction
Recently, the first catheter ablation of AVNRT had been reported in a patient with the combination of an anomalous IVC with azygos continuation and a PLSVC. They used non-fluoroscopic navigation systems in the ablation procedures. However, we could perform successful catheter ablation of AVNRT with conventional fluoroscopy guidance, without aids of navigation systems.
Case
A 40-year-old female patient was referred to our hospital for ablation of recurrent episodes of reentrant tachycardia. The chest X-ray was normal. The electrocardiogram obtained during the attack of her typical symptoms showed a narrow QRS complex, regular tachycardia, terminated with intravenous adenosine injection (Figure 1).
Echocardiography revealed a markedly enlarged CS, which suggested the presence of a PLSVC. Chest CT angiogram revealed interrupted IVC and azygos continuation to superior vena cava (Figure 2).
Cardiac electrophysiology study was performed after written informed consent. A CS catheter was introduced through the PLSVC from the left subclavian vein. Catheters for HRA, RV and His bundle area were introduced through the right superior vena cava and azygos vein from the femoral vein because the IVC was interrupted
(Figure 3).

Figure 1. ECG showed narrow QRS regular tachycardia of 150/min without visible P wave, suggesting AV nodal reentry tachycardia.

Figure 2. Chest CT angiogram revealed interrupted inferior vena cava and azygos continuation to superior vena cava (right posterior oblique view).
We used a deflectable catheter in order to record the His bundle potential and conventional quadripolar electrode catheters were located at HRA and RV. Rapid ventricular pacing demonstrated concentric retrograde atrial activation with decremental property. Supraventricular tachycardia was induced by single atrial premature depolarization after AH jump and the result of entrainment pacing was consistent with typical AVNRT.
After CS venogram (Figure 3A, 3B), we tried to map the slow pathway potential and precise
course of the His bundle. The slow pathway potential could not be mapped from that area. The His bundle potential was recorded at just above the roof of the dilated CS ostium. A deflectable 7 Fr ablation catheter was introduced through the azygos vein and right superior vena cava. Ablation was attempted from the bottom of CS ostium using anatomical approach. AVNRT was not able to be eliminated from the floor and mid part of CS ostium, although a junctional rhythm appeared during radiofrequency delivery. Atrioventricular
nodal dual physiology was eliminated by positioning the ablation catheter more anteriorly inside the very proximal CS (Figure 3C, 3D).
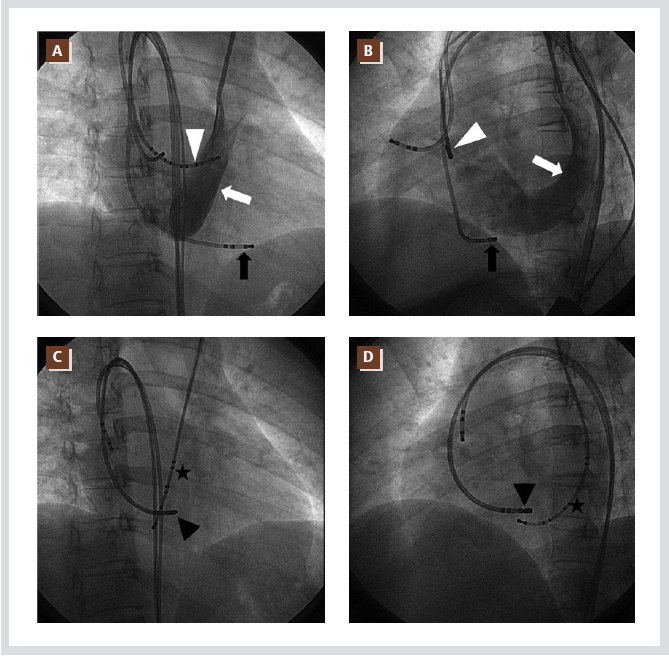
Figure 3. Coronary sinus venogram showed a huge dilated coronary sinus (white arrows: coronary sinus, white arrow heads: His catheter, A: RAO view, B: LAO view). Coronary sinus catheter was introduced through a persistent left superior vena cava from the left subclavian vein. Catheters for right atrium, right ventricle and His bundle were introduced through the azygos vein and superior vena cava from both femoral veins because of the interruption of IVC (black arrow heads: ablation catheter, stars: coronary sinus
catheter, C: RAO view, D: LAO view).
Junctional rhythm appeared again during radiofrequency delivery. Afterward, no AH jumps or atrioventricular nodal echoes were induced at baseline state nor during isoproterenol infusion. The patient was discharged without any complications. The patient has been well without recurrence of the tachycardia.
Thus, we performed a successful catheter ablation of AVNRT in a patient with combined congenital anomaly of an interrupted IVC with azygos continuation and a PLSVC.
Discussion
The malformations of the systemic venous connection to the heart may be summarized as follows: (a) Left superior vena cava connected to the CS, interrupted IVC and absent right superior vena cava; (b) Left superior vena cava connected to the left atrium, due to incorporation of the CS into the left atrial cavity; (c) Right superior vena cava or IVC draining into the left atrium; (d) Total anomalous systemic venous connection to the left atrium, usually combined with atrial isomerism; (e) Cor triatriatum
dexter.1
Persistent left superior vena cava is a relatively common anomaly of the systemic venous system, with an incidence of 0.3~0.5% in the general population. This incidence is higher in patients with congenital heart disease and in patients with atrioventricular connection abnormalities.2
Prevalence of interrupted IVC is 0.6~2.0% in patients with congenital heart disease and less than 0.3% among otherwise normal patients.3
To the best of our knowledge, the first catheter ablation of AVNRT had been reported in a patient with the combination of an anomalous IVC with azygos continuation and a PLSVC like our case by Arias et al recently.4 They used non-fluoroscopic navigation systems in the ablation procedures. However in our case, successful catheter ablation was performed with conventional fluoroscopy
guidance at the anterior portion of the proximal coronary sinus. Sakabe et al.5 reported successful ablation at posteroinferior region of Koch’s triangle with anatomical approach. Such variations of successful sites might be due to various course of the atrioventricular nodal slow pathway in patients with PLSVC, which might be affected by the dilated CS ostium due to PLSVC.5
Of note, catheter ablation of AVNRT in patients with a PLSVC requires more careful attention to avoid the risk for atrioventricular block,
because of the extraordinary anatomy of Koch’s triangle and the unusual course of the His bundle due to the huge dilation of the CS ostium.
References
- Mazzucco A, Bortolotti U, Stellin G, Gallucci V. Anomalies of the systemic venous return: a review. J Card Surg. 1990; 5:122-133.
- Katsivas A, Koutouzis M, Nikolidakis S, Lazaris E, Arealis G, Kyriakides ZS. Persistent left superior vena cava associated with common type AV nodal reentrant tachycardia and AV reentrant tachycardia due to concealed left lateral accessory pathway. Int J Cardiol. 2006;113:E124-125.
- Timmers GJ, Falke TH, Rauwerda JA, Huijgens PC. Deep vein thrombosis as a presenting symptom of congenital interruption of the inferior vena cava. Int J Clin Pract. 1999;53:75-76.
- Arias MA, Castellanos E, Puchol A, Valverde I, Pachon M, Garcia-Cosio MD, Rodriguez-Padial L. Atrioventricular nodal tachycardia in a patient with anomalous inferior vena cava with azygos continuation and persistent left superior vena cava. Pacing Clin Electrophysiol. 2009;32:1357-1358.
- Sakabe K, Fukuda N, Wakayama K, Nada T, Shinohara H, Tamura Y. Radiofrequency catheter ablation for atrioventricular nodal reentrant tachycardia in a patient with persistent leftsuperior vena cava. Int J Cardiol. 2004;95:355-357.
|