|
|
International Journal of Arrhythmia 2011;12(4): 16-23.
|

What is rhythm discrimination?
The term rhythm discrimination is generally used
to describe the ability of an implantable
cardioverter-defibrillator (ICD) to distinguish
between tachyarrhythmias that the device should
treat and other detected rhythms for which therapy
should not be delivered. In practice, defining what
should and should not be treated is as much a
matter of philosophy as it is a technological issue.
The transition from secondary prevention indications to primary prevention implants, and the
related changes in clinicians’ and patients’
attitudes over the years have further complicated
the matter.
In the discussion that follows, the authors review
the discrimination features and algorithms
available in current ICD systems, and highlight the
choices faced by the practitioner when deciding
what to treat and what to consider when
programming an ICD system to achieve the desired
results. The potential for future enhancements will
also be discussed.
Basic building blocks of ICD rhythm
discrimination
When a clinician looks at an ECG or intracardiac
electrogram (IEGM) to evaluate a rhythm, he or she
usually considers a variety of factors, such as:
How fast is the rhythm?
Is the rhythm sustained?
What is the relationship between atrial and
ventricular events? Is there synchrony or
dyssynchrony? Is every P-wave associated with
an R-wave? Is the timing between P-waves and
R-waves relatively constant? Is there a
consistent pattern?
How did it start? Was the onset abrupt? Was it
initiated by a premature ventricular contraction
(PVC) or a premature atrial contraction (PAC)?
Is the ventricular rate regular or irregular?
How do the R-waves look? Do they look like Rwaves
during sinus rhythm, or different?
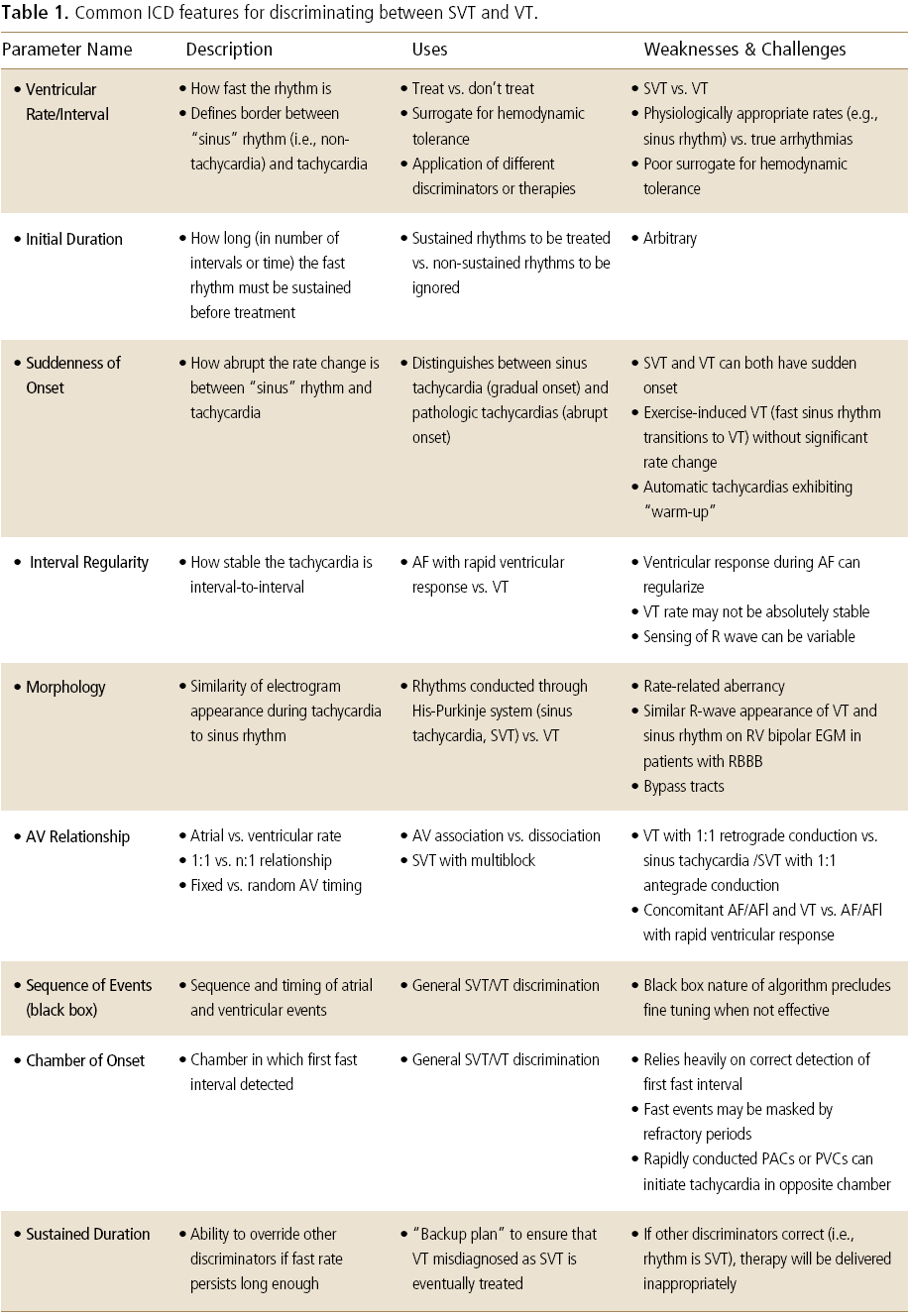
Today’s ICDs use features and algorithms that
attempt to mimic the clinicians’analytic approach
by attempting to answer these same questions.
These features and algorithms, which are
summarized in Table 1, are well known to
practitioners who regularly program ICDs, and will
not be discussed in detail here. Dual-chamber ICDs,
because they allow for the assessment of atrial
activity and the atrioventricular (AV) relationship,
provide an enhanced ability to distinguish
supraventricular tachycardia (SVT) from
ventricular tachycardia (VT). A schematic example
of how atrial activity and the AV relationship could
be integrated with the earlier discriminators is
shown in Figure 1.
Some ICD systems provide nearly infinite
programmability of each of the component features
of their discrimination algorithms. This enables the
system to be customized to the specific needs of an
individual patient, which may be particularly useful
when inappropriate therapies are delivered because
of atypical combinations of events. The system can
be confusing to program, however, particularly for
primary prevention patients, where nothing is
known a priori about the characteristics of the
patient’s tachyarrhythmias. Other ICD systems
seek to minimize the programming complexity by
creating ‘black box’algorithms. As the term
implies, the workings of these algorithms are
largely hidden from the user, and there may be
little programmability beyond the ability to turn
them on or off. They are simple to use, and they
work well most of the time, but there is little
recourse when they do not. ICD manufacturers are
continually seeking to improve the user interfaces
on their programmers in order to reach an ideal
compromise: an on/off feature that works well most
of the time, combined with the ability to
troubleshoot and fine-tune the algorithm when
patient conditions dictate that adjustments be
made.
What rhythms are we trying to
discriminate between?
When the earliest ICDs were implanted, the
philosophy implicit in the approach to detection and
discrimination was simple: when in doubt, shock.
Because these were patients who had already
experienced at least one episode of arrhythmic
sudden cardiac death (SCD) or had documented VT
or ventricular fibrillation (VF), every instance in
which a shock was withheld in the face of a fast
rhythm presented the risk of failing to treat a
potentially lethal arrhythmia. For this reason, these
devices required only simple detection and
discrimination strategies and were designed with
What rhythms are we trying to
discriminate between?
When the earliest ICDs were implanted, the
philosophy implicit in the approach to detection and
discrimination was simple: when in doubt, shock.
Because these were patients who had already
experienced at least one episode of arrhythmic
sudden cardiac death (SCD) or had documented VT
or ventricular fibrillation (VF), every instance in
which a shock was withheld in the face of a fast
rhythm presented the risk of failing to treat a
potentially lethal arrhythmia. For this reason, these
devices required only simple detection and
discrimination strategies and were designed with the philosophy of ‘better a few shocks too many
than one shock too few’. With the advent of tieredtherapy
devices, which delivered antitachycardia
pacing (ATP) and cardioversion shocks to treat
slower, potentially better-tolerated VTs in addition
to hemodynamically unstable VT and VF, it became
desirable to be able to differentiate between VT and
VF, and also between rapid ventricular rates due to
ventricular arrhythmias and those associated with
SVT. Today, most ICDs are implanted for primary
prevention (i.e., prophylactically). Therefore, in
patients who are not as keenly aware of the need
for their ICD implantation, the tolerance for
inappropriate or unnecessary shocks has
diminished. The result has been a renewed
emphasis on the development of algorithms and
programming strategies that will result in the
delivery of ICD therapy, and shocks in particular,
only when absolutely necessary. Thus, for today’s
primary prevention patient, the implicit philosophy
can be summarized as ‘better one shock too few
rather than a few too many’.
The challenge in designing and programming ICD
discrimination algorithms is that it is not always
clear which rhythms are appropriate to treat, and
with what therapy. Many different factors must be
considered when deciding what device behavior is
appropriate and necessary, and this decision may
differ from patient to patient, and from physician
to physician. Some key considerations in the
decision-making process are as follows:

Future Generations of the ICD
The current state of the art in ICD packaging has
reached technological maturity. Increased miniaturization
will probably yield just a marginal decrease in the
overall displacement volume of the device, which
will be accompanied by a significant increase in
manufacturing cost. The cost of the precious metals
used in the device continues to rise. Because the
ICD has a number of components that are unique to
its application, it is doubtful that the current
advances being made in the high volume personal
electronics revolution would be of use in reducing
its size and cost.
If the clinical requirements for an ICD could be
modified or relaxed, it would be possible to conceive
of a new generation of devices that are smaller and
that cost less. Relaxation of the design constraints
could lead to the modification or complete
elimination of the components within the ICD.
Special batteries, high voltage capacitors, and high
voltage output circuits could become smaller and
less costly to manufacture.
The first example of a future generation ICD is one that allows for a significant increase in its
charge time in preparation for the delivery of
therapy to the patient. The device would charge at
a lower input power. A reduction in the maximum
target charging voltage would make possible a
significant reduction in the size of the device
circuits and their respective components. In this
case, alternative battery chemistries could be
employed, such as Carbon Monofluoride (CFx). The
size of the battery, the high voltage capacitor set,
and the high voltage output circuit could also be
reduced, bringing about a significant cost reduction
as well. It is recognized that this new ICD may not
be suitable for all patients.
The second example of a future generation ICD is
one that is more disruptive and unconventional in
its design approach. This device is able to sense and
detect tachyarrhythmias just before their onset.
One class of therapy regime would consist of low
voltage pace trains that would decelerate the
arrhythmia into a normal sinus rhythm.2 Another
class of therapy regime would stimulate the
autonomic nervous system via thoracic spinal cord
stimulation in a way that would prevent the onset
of an arrhythmia.4 This new generation of devices
has the function of a low voltage implantable pulse
generator, and it looks more like a pacemaker or a
spinal cord stimulator. It would make possible a
significant size and cost reduction relative to the
design of the conventional ICD.
Is it SVT or VT?
In the era when ICDs were predominantly
implanted for secondary prevention, there was
general agreement in the device community that
every episode of VT or VF should be treated, and
that every shock delivered for anything other than
VT or VF was inappropriate. The discrimination
algorithms of this era, then, which were largely
based on the features listed in Table 1, were
generally effective in making these distinctions, but
were known and are known to be less than perfect.
Because the predominant philosophy was that it
was unacceptable to miss even a single episode of
VT, when the device was unsure whether a rhythm
was SVT or VT (for example, when different
discriminators reached different conclusions), the
algorithms were biased towards overtreatment,
with the result that patients received inappropriate
shocks (i.e., shocks for rhythms other than VT or
VF). Recent studies1,2 estimate that approximately
20% of ICD patients receive inappropriate shocks within three years of receiving an implant.
Is a Shock Necessary?
As more patients receive their ICDs for primary
prevention, and because of concerns that the
shocks themselves may negatively affect their
survival, the delivery of shocks has become less
acceptable to patients and clinicians. This has led to
a distinction between appropriate shocks (i.e.,
shock delivered as a result of a correct device
diagnosis of VT or VF) and necessary shocks (i.e.,
shocks delivered only when shocks are the best
alternative).
Until recently, most ICDs were programmed with
relatively low VT detection rates (often in the range
of 150-160 bpm) and relatively short detection
durations (typically 10-15 intervals) Any VT that
remained above the programmed detection rate for
the programmed duration and met any other
programmed discrimination criteria would cause
the device to deliver therapy, most often in the
form of a shock. Several studies have shown,
however, that for primary prevention patients,
many shocks can be avoided by employing
alternative programming strategies.3,4,5,6 First, these
studies demonstrated that many VT episodes
would self-terminate (i.e., without any device
intervention) if they were allowed more time (up to
30-40 intervals) to run their course. Second, the
studies showed that the VT detection rate could be
programmed significantly faster (up to a range of
180-190 bpm) without compromising the patient’s
safety. Finally, the studies demonstrated that a
single burst of ATP could be very effective in
terminating even fast VTs. This combination of
higher detection rates, longer detection times, and
at least one ATP burst has been shown to reduce
the number of delivered shocks by as much as 50%.
As a result, many experts are now advocating that
clinicians adopt a default programming strategy
based on the parameters that were shown to be
effective in these studies. Thus, the philosophy has
begun to evolve from, ‘The ICD must terminate
every episode of VT’, to ‘The ICD is meant to
prevent sudden death, not to treat non-lethal
rhythms’. Several manufacturers have recently
revised their default parameters to better reflect
this change in indications and attitudes, and the
analyses7,8 indicate that these revised parameters
may dramatically reduce the number of
inappropriate and unnecessary shocks.
Is the Device Correctly Detecting
R-Waves and P-Waves?
ICD rhythm discrimination is predicated on the
assumption that the device accurately senses Rwaves,
and that in the case of dual-chamber ICDs,
it detects P-waves as well, despite the fact that the
signal amplitudes may vary by more than one order
of magnitude as the patient’s rhythm transitions
between sinus rhythm, tachycardia, and
fibrillation. In addition, the device must not be
prone to oversensing anything other than R-waves
on the ventricular lead, and P-waves on the atrial
lead, whether they are of physiological or nonphysiological
origin. To ensure proper sensing, all
modern ICDs employ bipolar sensing, either
between closely-spaced tip and ring electrodes
(standard bipolar configuration) or between a tip
electrode and the right ventricular shock coil
(integrated bipolar configuration). They also employ
sophisticated automatic gain control or automatic
sensitivity control algorithms in the ventricle (and,
in some cases, in the atrium) that rapidly adapt to
changes in signal amplitude, and frequency filters
designed to optimize the sensing of R-waves, Pwaves,
and fibrillation, and to minimize the sensing
of physiological signals such as T-waves and
myopotentials, and the sensing of nonphysiological
signals from various external
electromagnetic sources.
Noise generated by failing leads (either due to
breaches of a lead’s insulation or breaks in the
conductor wires) remains a troubling complication
of the sensing function. This often manifests as
oversensing, which results in the delivery of
inappropriate shocks, which, in the worst case, may
occur in clusters.9 While this was once considered
an unfortunate but unavoidable side effect of lead
failure, recent attention to this problem from ICD
manufacturers has led to advances that promise to
aid in the earlier detection of such lead-related
oversensing, thereby reducing the number of
inappropriate shocks that occur.
What Does the Future Hold?
As in every other aspect of ICD technology, ICD
rhythm discrimination will continue to evolve.
While it is impossible to predict exactly what
changes will be successfully implemented, certain
technological trends seem likely to have a positive
impact on the ICD’s ability to discriminate. Three of
the most promising trends are as follows:
More processing power coupled with more
memory: This will result in smarter, more
powerful systems that can incorporate more
sophisticated signal processing, which could
facilitate the development of advanced
algorithms that could self-learn and adapt to
changes in a patient’s condition or physiology, or
could better deal with the incomplete or
conflicting data that the ICD must use to make
its decisions.
Hemodynamic sensing: An ideal discrimination
system would be able to distinguish between
hemodynamically stable and unstable rhythms,
and make treatment decisions accordingly.
Today’s devices use the rate as a surrogate for
hemodynamic tolerance, which allows
discrimination and therapy strategies to be
applied differently to different rate zones, based
on the assumption that arrhythmias in slower
zones will be better tolerated and will present
less of a risk if they go untreated. Unfortunately,
the rate is a far-from-perfect indicator of
hemodynamic tolerance, both among multiple
patients and in the same patient at various times and
under various conditions. Today, hemodynamic
sensors are being integrated into ICD systems for
non-discrimination purposes, such as for the
detection of the onset of acute heart failure
decompensation. It is thus entirely possible, and
even likely, that they will eventually be
evaluated for their ability to determine
hemodynamic tolerance.
Integration of relevant patient data into device
operations: As the data from devices is merged
into electronic health records, the relationship
between changes in a patient’s condition and
treatment and their effect(s) on the device data
could be analyzed. This would result in
suggestions for programming changes that
would optimize the device performance as well as
patient outcomes.
Summary
Today ’s ICDs provide a wide range of programmable
parameters and sophisticated algorithms that
effectively discriminate between VT/VF and SVT,
and also prevent inappropriate detection and
therapy delivery due to the oversensing of
physiological and non-physiological signals.
Despite the availability of this advanced technology, or perhaps because of it, clinicians are
faced with the daunting task of programming these
systems to achieve goals that are sometimes
unclear. The ability to distinguish VT and VF from
every other manifestation, once considered the holy
grail of rhythm discrimination, is no longer
sufficient, particularly for patients who receive
their implants for primary prevention.
Philosophical decisions, including whether the
ultimate goal of ICD therapy is to treat every
ventricular arrhythmia or only to prevent sudden
death (or, stated another way, whether it is ever
acceptable to not detect and treat a true VT), and
when shocks are not only appropriate but are
necessary, must be decided for each patient, and
the devices must be programmed accordingly. While
it is likely that future developments will enhance
these systems’technological capability to detect
and distinguish between various rhythms, these
advances are equally likely to raise new
philosophical issues that the clinician must wrestle
with.
Employee: Dr. Ostrow is a board member of
Clinical Advisory Group of St. Jude Medical
International.
References
- Kadish A, Dyer A, Daubert JP, Quigg R, Estes NA, Anderson KP, Calkins H, Hoch D, Goldberger J, Shalaby A, Sanders WE, Schaechter A, Levine JHfor the Defibrillators in Non-Ischemic Cardiomyopathy Treatment Evaluation (DEFINITE) Investigators. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy.
N Engl J Med .
2005; 350(21):2151-2158.
- Poole JE, Johnson GW, Hellkamp AS, Anderson J, Callans DJ, Raitt MH, Reddy RK, Marchlinski FE, Yee R, Guarnieri T, Talajic M, Wilber DJ, Fishbein DP, Packer DL, Mark DB, Lee KL, Bardy GH. Prognostic importance of defibrillator shock in patients with heart failure.
N Engl J Med.
2008;359:1009-1017.
- Wathen MS, DeGroot PJ, Sweeney MO, Stark AJ, Otterness MF, Adkisson WO, Canby RC, Khalighi K, Machado C, Rubenstein DS, Volosin KJ; PainFREE Rx II Investigators. Prospective randomized multicenter trial of empirical antitachycardia pacing versus shocks for spontaneous rapid ventricular tachycardia in patients with implantable cardioverter-defibrillators: Pacing Fast Ventricular Tachycardia Reduces Shock therapies (PainFREE Rx II) trial results.
Circulation.
2004;110:2591-2596.
- Wilkoff BL, Ousdigian KT, Sterns LD, Wang ZJ, Wilson RD, Morgan JM; EMPIRIC Trial Investigators.A comparison of EMpiric to Physician-tailored progRamming of Implantable Cardioverter-defibrillators: results from the prospective randomized multicenter EMPIRIC trial.
J Am Coll Cardiol.
2006;48:330-339.
- Wilkoff BL, Williamson BD, Stern RS, Moore SL, Lu F, Lee SW, Birgersdotter-Green UM, Wathen MS, Van Gelder IC, Heubner BM, Brown ML, Holloman KK for the PREPARE Study Investigators. Strategic programming of detection and therapy parameters in implantable cardioverter-defibrillators reduces shocks in primary prevention patients.
J Am Coll Cardio .
2008;52:541-550.
- Gasparini M, Menozzi C, Proclemer A, Landolina M, Iacopino S, Carboni A, Lombardo E, Regoli F, Biffi M, Burrone V, Denaro A, Boriani G. A simplified biventricular defibrillator with fixed long detection intervals reduces implantable cardioverter defibrillator (ICD) interventions and heart failure hospitalizations in patients with non-ischaemic cardiomyopathy implanted for primary prevention: the RELEVANT [Role of long dEtection window programming in patients with LEft VentriculAr dysfunction, Non-ischemic eTiology in primary prevention treated with a biventricular ICD] study.
Eur Heart J.
2009;30:2758-2767.
- Deering TF, Epstein AE, Greenberg SM, et al. Performance of optimized SVT discriminators and detection rates in reducing total and inappropriate shocks.
Heart Rhythm.
2011;8:AB26-2 (abstract).
- Exner DV, Wathen MS, Volosin KJ, Sherfesee L, Scinicariello AP, Gillberg JM, University of Calgary, Libin Cardiovascular Institute of Alberta, Calgary, AB, Canada, None, Nashville, TN, Philadelphia Heart Institute, University of Pennsylvania, Philadelphia, PA, Medtronic Inc., Minneapolis, MN. Time course and characterization of defibrillator shocks using a virtual ICD model.
Heart Rhythm.
2010;7:P02-129 (abstract).
- Krahn AD, Champagne J, Healey JS, Cameron D, Simpson CS, Thibault B, Mangat I, Tung S, Sterns L, Birnie DH, Exner DV, Parkash R, Sivakumaran S, Davies T, Coutu B, Crystal E, Wolfe K, Verma A, Stephenson EA, Sanatani S, Gow R, Connors S, Paredes FA, Essebag V; Canadian Heart Rhythm Society Device Advisory Committee. Outcome of the Fidelis implantable cardioverter-defibrillator lead advisory: a report from the Canadian Heart Rhythm Society Device Advisory Committee.
Heart Rhythm.
2008;5:639-642.
|
|
|
|