|
|
International Journal of Arrhythmia 2012;13(3): 35-40.
|
 |
| ECG & EP CASES |
Surgical Ablation of
a Manifest Right Free Wall
Accessory Pathway |
 |
 |
Jae-Sun Uhm, MD1, Moon-Hyoung Lee, MD1, Byung-Chul Chang, MD2, Sung Soon Kim, MD3
1Division of Cardiology, 2Division of Cardiovascular Surgery, Severance Cardiovascular Hospital, Yonsei University College of Medicine
3Department of Cardiology, Armed Forces Capital Hospital
|
|
 |
 |
Introduction
Catheter ablation of an accessory pathway at the
right free wall is sometimes challenging because it
is difficult to maintain stable tissue contact with
the catheter and because the anatomy of this region
is complex. Here, we report the case of a patient
with Wolff-Parkinson-White (WPW) syndrome due
to a manifest right free wall accessory pathway
that was surgically ablated.
Case
A 20-year-old male patient with abrupt-onset
palpitations and dyspnea while running was
referred to our hospital after being admitted to the
emergency room, 1 week ago. The patient had a
single episode of syncope several years before.
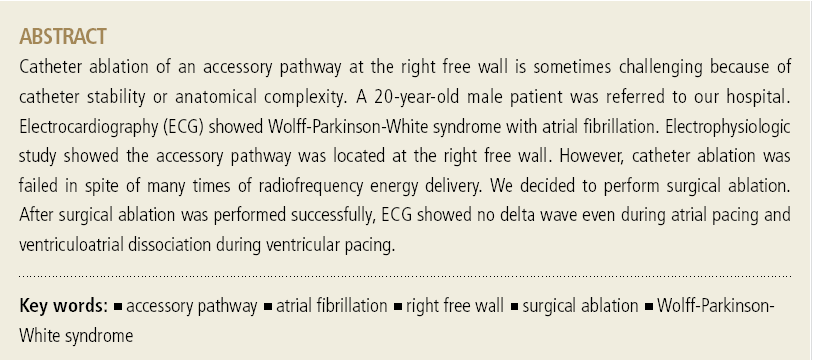
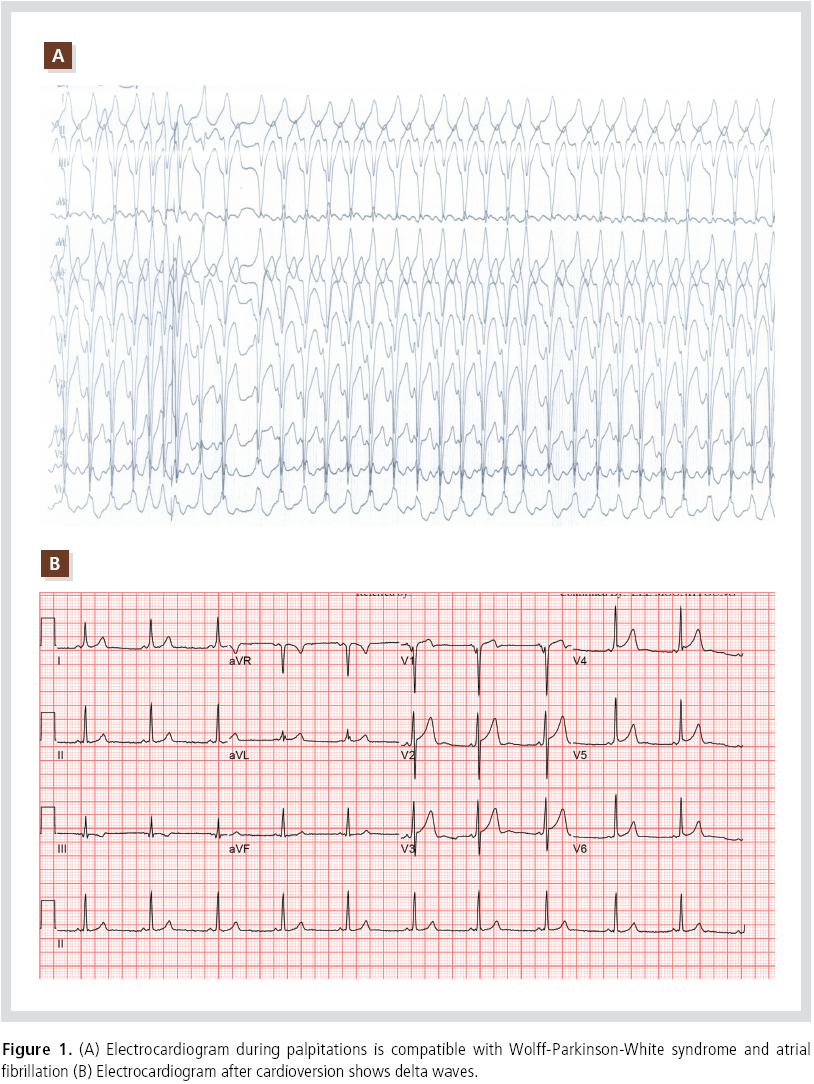
Electrocardiogram (ECG) showed wide QRS
tachycardia, irregularly irregular RR interval, and
multiple QRS morphology (Figure 1A). ECG was
compatible with atrial fibrillation in a patient with
WPW syndrome. Flecainide was administrated
intravenously for chemical cardioversion, after
atrial fibrillation converted to a normal sinus
rhythm, delta waves were apparent (Figure 1B).
Because the polarity of the delta wave in lead V1
was negative, it was possible that the manifest accessory pathway was located at the tricuspid
annulus. Physical examination, chest X-ray, and echocardiography did not show any abnormal
findings.
An electrophysiology study was performed with 3
quadripolar catheters placed in the lateral wall of
the high right atrium (HRA), His bundle area, and
right ventricular (RV) apex via the left femoral
vein. In addition, a decapolar catheter was threaded
into the coronary sinus via the right internal
jugular vein. Sinus rhythm was evident with AH
and HV intervals of 55 and 20 msec, respectively.
During ventricular pacing, eccentric retrograde
atrial activation was observed, with the earliest
atrial signal located at HRA electrodes 3,4. When
single ventricular premature extrastimuli were
delivered, ventriculoatrial (VA) conduction did not
have any decremental property. During atrial
pacing, delta waves and ventricular preexcitation
were augmented. When single atrial premature
extrastimuli were delivered, atrioventricular (AV)
conduction did not have any decrement. Narrow
QRS tachycardia was induced spontaneously with a cycle length of 352 msec. The RP interval was
shorter than the PR interval, and the VA interval
was 105 msec in duration. Intracardiac electrogram
showed eccentric retrograde right atrial activation
with the earliest atrial activation at the HRA
electrode pair 3,4 (Figure 2). This was compatible
with orthodromic atrioventricular reentrant
tachycardia resulting from a right free wall
accessory pathway. Meticulous retrograde and
antegrade mapping around the right free wall/
tricuspid annulus was performed with an ablation
catheter (EP Technologies, Natick, MA, USA). The
narrowest VA conduction signals and accessory
pathway signal were found at the 8-o'clock position
on the tricuspid annulus. We determined this was
the location of the accessory pathway, and
radiofrequency energy of up to 50 Watts and 50℃
was delivered to the site with the ablation catheter
in a Mullin sheath(Figure 3). After 30 ablation attempts, the accessory pathway persisted, although
ECG and intracardiac electrogram showed transient
loss of delta waves during radiofrequency energy
delivery. We presumed the accessory pathway was
located deep within the tricuspid annulus and
decided upon surgical ablation as the best course of
action.


The next day the patient was transferred to the
operating room for surgical ablation. The ablation
of right free wall and right posterior accessory
pathway was approached via median sternotomy
and right atriotomy under the total cardiopulmonary
bypass. Atrial side of the right free wall,
4-5 mm from the tricuspid annulus was incised and
dissected to the epicardial reflection of the right
ventricle after cardioplegia (Figure 4). At the end of
the incision adjacent to the AV node, endocardium
was incised and dissected under beating heart to
prevent AV node injury. Finally, cryolesion was made at the AV nodal area after release of aorta
cross clamping and the endocardial incision was
sutured continuously. After surgical ablation and
weaning of the cardiopulmonary bypass pump, ECG
showed no delta wave (Figure 5). Before closing the
sternum, 2 pacing wires were implanted on the
right atrial and RV free wall in case of postoperative
AV block. Atrial pacing was performed postoperatively
with the pacing wire, and no delta waves
were observed. The patient was discharged without
complication, and a follow-up visit to the outpatient
clinic did not show any evidence of recurrence.
Discussion
In 1968, Rosenbaum and his colleagues described
Catheter ablation of right-sided accessory
pathways is sometimes challenging because of
catheter instability and anatomical complexities of
the tricuspid annulus.1 A Schwartz right or Mullin sheath can be useful for right free wall ablations. It
aids approach by making a large loop around the
tricuspid annulus with the ablation catheter.
Recent reports have noted that three-dimensional
electroanatomical mapping systems and remote
robotic systems can also be used successfully for
catheter ablation of right-sided accessory
pathways.2,3

In the present case, because of
anatomical complexities and because the accessory
pathway was located deep within the tricuspid
annulus, catheter ablation could not be succeed.
Although surgical ablation is less prevalent now
because of recent developments in catheter ablation
techniques and equipment, it remains a useful tool
in cases like those described here.
References
- Jackman WM, Wang X, Friday KJ, Roman CA, Moulton KP,
Beckman KM, McClelland JH, Twidale N, Hazlitt HA, Prior MI,
Margolis PD, Calame JD, Overholt ED, Lazzara R. Catheter
ablation of accessory atrioventricular pathways (Wolff-Parkinson-
White syndrome) by radiofrequency current.
N Engl J Med.
1991;324:1605-1611.
- Long DY, Dong JZ, Liu XP, Tang RB, Ming M, Gao LY, Yu RH,
Fang DP, Jiang CX, Yuan YQ, Sang CH, Yin XD, Chen G, Zhang
XY, Liang C, Ma CS. Ablation of right-sided accessory pathways
with atrial insertion far from the tricuspid annulus using an
electroanatomical mapping system.
J Cardiovasc Electrophysiol.
2011;22:499-505.
- Steinwender C, Honig S, Leisch F, Hofmann R. Ablation of a
right-sided accessory pathway with the Hansen robotic system.
Europace.
2011;13:755-756.
|
|
|
|