|
|
International Journal of Arrhythmia 2013;14(3): 28-33.
|
Introduction
Steam pops are infrequent in radiofrequency
(RF) ablation for ventricular tachycardia (VT);
although they have been reported to occur in
only 1~1.5% of all RF ablations, they can cause
cardiac tamponade, especially in the right ventricular
outflow tract (RVOT).1-3
Case Report
A 57-year-old woman presented to our emergency department with a 1-week history of waxing
and waning palpitations that worsened and
persisted on the day of admission, with associated
dizziness and chest discomfort. Hypertension
had been diagnosed 2 years earlier and was controlled
by an angiotensin receptor blocker. Her
family and social history were unremarkable. Her
initial blood pressure (BP) was 130/98 mmHg,
with a pulse rate of 170 beats/min and a respiration
rate of 22 breaths/min. Her electrocardiogram
showed a wide QRS tachycardia with left
bundle branch block morphology, inferior axis,
QRS width >140 ms, aVL size slightly greater
than aVR, and a small r wave of >0.2 mV in the
V2 lead, which suggested that the tachycardia
originated from the left superior free wall of the
RVOT (Figure 1).

Rapid administration of intravenous
adenosine and slowly repeated infusions
of diltiazem and verapamil had no effect. After sedation, biphasic direct cardioversion (50 J) was
performed twice; however, the tachycardia continued,
and her BP dropped to 70/56 mmHg. A
flecainide infusion was started, and the tachycardia stopped during that infusion. Laboratory
test results were within normal limits, and
a transthoracic echocardiogram showed normal
left ventricular ejection fraction (64%) and mild mitral regurgitation (grade I). The next day, an electrophysiology
study was performed. With the patient
fasting and unsedated, a 6 Fr quadripolar catheter
was placed in the right ventricular (RV) apex and
a 7 Fr deflectable non-irrigation catheter (CelsiusTM,
Biosense Webster, Diamond Bar, CA, USA) via an
SR-0 sheath (St. Jude Medical, St. Paul, MN, USA)
was placed in the RVOT via the right femoral vein.
After performing an angiogram of the RVOT area, 3D
electroanatomic mapping (EnsiteTM, St. Jude Medical)
was performed. The baseline rhythm was sinus with
occasional ventricular premature contractions (VPC),
whose morphology was compatible with the clinical
VT. VT originating from the RVOT (cycle length 400
ms) was repeatedly induced by the RV burst pacing.
The earliest ventricular potential was recorded at the
left-superior area between the free wall and septum
of the RVOT, and pace-mapping showed an identical
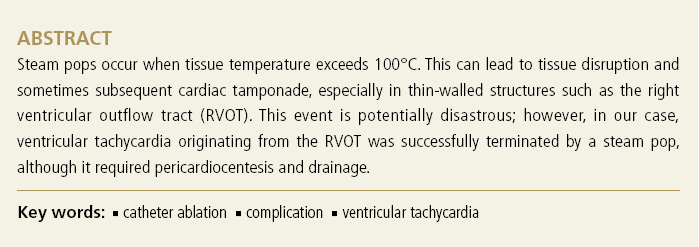
VT morphology. The presystolic potential at the
ablation catheter was earlier than the surface QRS onset at lead V2 by approximately 22 ms, and the 3D
mapping point was compatible with the point. During
RF ablation at the point on the VT state, VT was
successfully terminated (Figures 2 and 3).
However,
some VPCs and non-sustained VTs remained after
several additional ablations, which might have been
associated with improper power delivery because of
impedances and temperature limitations. Therefore,
we changed the ablation catheter to a 7 Fr unidirectional
irrigated form (CelsiusTM Thermocool®, Biosense
Webster) for increased power delivery. RF ablation
(45 W, with the maximum catheter tip temperature
set to 50°C) was repeated at the same ablated
site. Catheter irrigation was started automatically at
a flow rate of 30 mL/min at the start of the ablation.
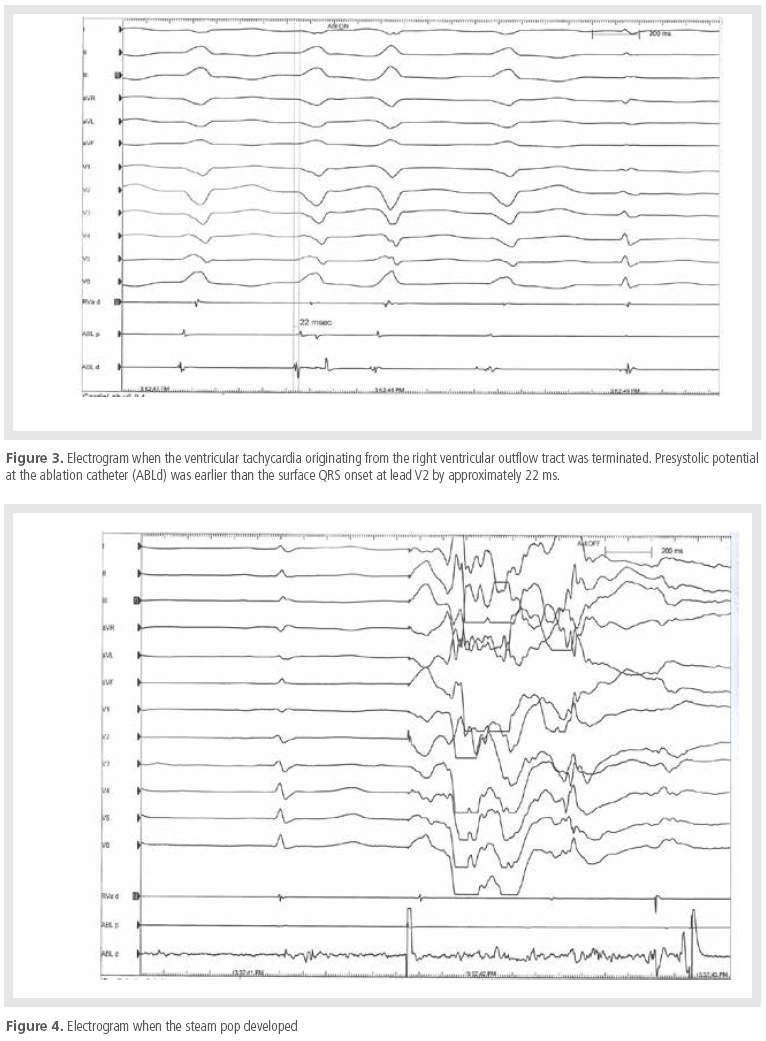
During ablation, a sudden audible steam pop
developed (Figure 4).

Energy delivery was immediately
stopped after the pop occurred. However, the
patient’s BP suddenly dropped and she became stuporous.
After confirmation of cardiac tamponade by portable transthoracic echocardiography, pericardiocentesis
with drainage was performed. After
drainage, the patient’s BP improved to 100/70
mmHg. Fortunately, after this event, no more
VPCs or VTs were observed for >30 min (Figure
5). We finished the procedure, keeping the pericardial
drainage in place. After 3 days of supportive
care, she was discharged. There were no
further events over the 2-year follow-up period.
Discussion
RF ablation causes lesion development by inducing
cell death when tissue temperature exceeds
50°C; however, it can also cause steam
pops when the tissue temperature is >100°C,
sometimes far exceeding the catheter tip temperature.1,3 When steam explosions occur, which
maybe audible as steam pops, they can cause
cardiac perforation. This dangerous situation
occurs more commonly in the RV than in the
left ventricle because of the thin-walled structure
of the RV.2,4 Externally irrigated RF ablation
can cool the catheter-tissue interface, making
it possible to increase power delivery and reduce
coagulum formation. However, irrigated RF also
causes an imbalance between tissue and catheter
tip temperatures during ablation, causing difficulty
in predicting steam pops.3 Cooper et al.
found a relationship between pops and electrode
temperature during atrial ablation and recommended
maintaining a catheter tip temperature
<40°C to prevent steam pops.5 However, steam
pops were observed when the mean catheter tip
temperature was 39°C with open irrigation and
even occurred with catheter tip temperatures as
low as 34°C.1 Yokoyama et al. demonstrated that
steam pops occurred more frequently as power
was increased from 30 to 50 W.6 Hsu et al. suggested
that pops occurred when power exceeded
48 W, and pop formation was limited when power
remained under 42 W.7 However, Seiler et al.
showed no significant difference between power
settings for lesions with and without pops, and
found that limiting RF power to achieve an impedance
decrease of <18 Ω is a feasible method
of reducing steam pops.1 Nonetheless, higher
maximum energies and larger impedance falls
are associated with steam pops.4 Koruth et al.
demonstrated that steam pops can be predicted
by the rate of temperature rise and the maximum
volumetric temperature measured by microwave
radiometry during irrigated RF ablation.3 Increasing
contact force also was proportionally
associated with more steam pops.8 In our case,
the relatively high power (45 W) and technically
increasing contact force may have been related
causes of the steam pops, but we could not check
the spike in impedance because of the unstable
situation. Whether the VT focus was abolished
by elevated RF power delivery or the steam pop,
the interpretation was tangled. Anyway careful
handling of the ablation catheter and monitoring
of impedance and catheter tip temperature,
and possibly a low power setting, is required to
prevent steam pops.
References
- Seiler J, Roberts-Thomson KC, Raymond JM, Vest J, Delacretaz
E, Stevenson WG. Steam pops during irrigated radiofrequency
ablation: feasibility of impedance monitoring for prevention.
Heart Rhythm.
2008;5:1411-1416.
- Tokuda M, Kojodjojo P, Epstein LM, Koplan BA, Michaud GF, Tedrow
UB, Stevenson WG, John RM. Outcomes of cardiac perforation
complicating catheter ablation of ventricular arrhythmias.
Circ Arrhythm Electrophysiol.
2011;4:660-666.
- Koruth JS, Dukkipati S, Gangireddy S, McCarthy J, Spencer D,
Weinberg AD, Miller MA, D'Avila A, Reddy VY. Occurrence of Steam Pops During Irrigated RF Ablation: Novel Insights from
Microwave Radiometry.
J Cardiovasc Electrophysiol.
2013 [Epub ahead of print].
- Tokuda M, Tedrow UB, Stevenson WG. Silent steam pop detected by
intracardiac echocardiography.
Heart Rhythm.
2012 [Epub ahead of print].
- Cooper JM, Sapp JL, Tedrow U, Pellegrini CP, Robinson D, Epstein
LM, Stevenson WG. Ablation with an internally irrigated
radiofrequency catheter: learning how to avoid steam pops.
Heart Rhythm.
2004;1:329-333.
- Yokoyama K, Nakagawa H, Wittkampf FH, Pitha JV, Lazzara R,
Jackman WM. Comparison of electrode cooling between internal and open irrigation in radiofrequency ablation lesion depth and
incidence of thrombus and steam pop.
Circulation
2006;113:11-19.
- Hsu LF, Jais P, Hocini M, Sanders P, Scavee C, Sacher F, Takahashi Y,
Rotter M, Pasquie JL, Clementy J, Haissaguerre M. Incidence and
prevention of cardiac tamponade complicating ablation for atrial
fibrillation.
Pacing Clin Electrophysiol.
2005;28 Suppl 1:S106-109.
- Yokoyama K, Nakagawa H, Shah DC, Lambert H, Leo G, Aeby N,
Ikeda A, Pitha JV, Sharma T, Lazzara R, Jackman WM. Novel contact
force sensor incorporated in irrigated radiofrequency ablation
catheter predicts lesion size and incidence of steam pop and
thrombus.
HCirc Arrhythm Electrophysiol.
2008;1:354-362.
|
|
|