|
|
International Journal of Arrhythmia 2014;15(1): 40-43.
|
Introduction
Recently, several studies documented a close association
between idiopathic VF (VF) and the presence
of early repolarization (ER) abnormalities in the
inferolateral leads. Dynamic change in the J wave
was frequently observed in patients with ER syndrome,
especially close to the arrhythmic event. We
report a case that presented with VF and temporal
evolution of the J wave.
Case
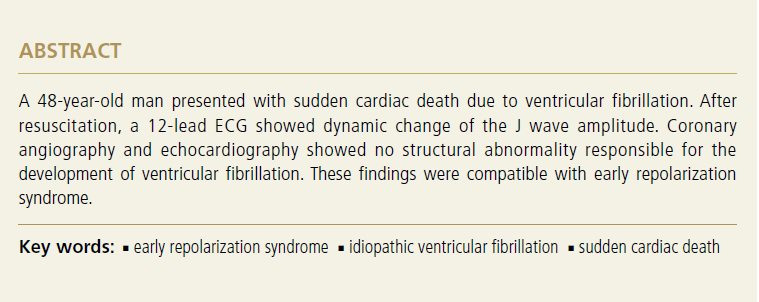
A 48-year-old man presented to emergency
medical service with sudden loss of consciousness.
He did not have a history of any relevant medical
illness. At emergency medical service arrival, the
patient was pulseless and an automated external
defibrillators (AED) recording obtained at the time
of the event showed VF (Figure 1). After successful
resuscitation by cardiac massage and a direct current
(DC) shock delivered by the Automated external
defibrillators, the patient was admitted to our hospital.
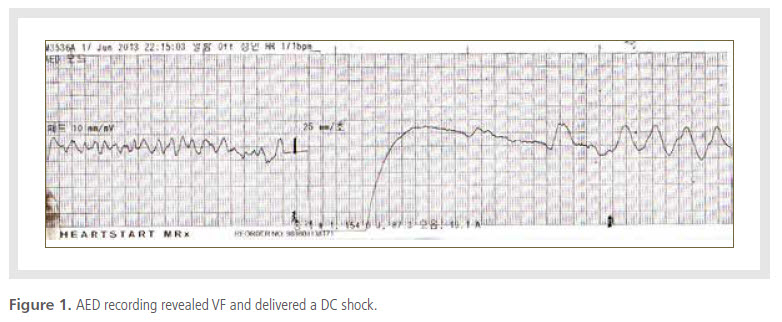
The 12-lead ECG obtained in the ER showed
no abnormal findings. However, a follow-up ECG
revealed dynamic change in the J-point amplitude
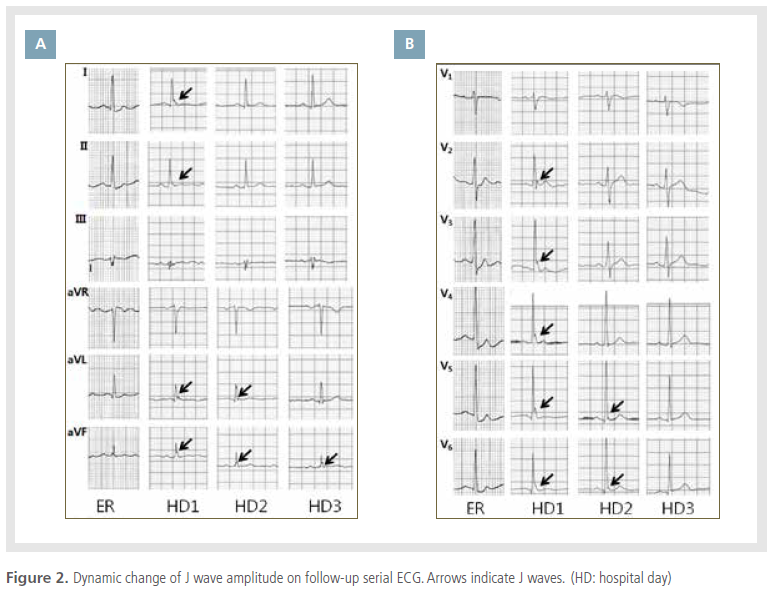
(Figure 2). During observation in the intensive care
unit, VF redeveloped subsequent to premature ventricular contractions with a very short cycle length
(Figure 3). After receiving advanced cardiac support,
the patient fully recovered without sequelae. Several
examinations including 2D echocardiography and coronary angiography showed no abnormal findings,
which enabled the exclusion of a secondary cause of
VF. An ICD was implanted in the patient for the secondary
prevention of sudden cardiac death (SCD) due to idiopathic VF.
Discussion
SCD is defined as an unexpected death from a cardiac
cause within a short period, generally ≤1 h from
symptom onset. The majority of SCDs are associated
with structural heart disease. Some individuals,
however, have a vulnerability for the development of
fatal arrhythmias caused by primary electrophysiological
abnormalities such as long QT syndrome and
Brugada symdrome.1-3
ER is a common electrocardiographic finding that
is generally considered benign. However, the presence
of this pattern, especially in the inferior or lateral
leads, has recently been recognized in some studies
to be associated with a vulnerability to VF.4-6 The
prognostic value of ER is nevertheless not completely
understood.
The ER pattern is characterized by J-point elevation
manifested either as QRS slurring (at the transition
from the QRS segment to the ST segment) or
notching (a positive deflection inscribed on the terminal
S wave), ST-segment elevation with upper concavity,
and prominent T waves in at least 2 contiguous
leads.
Dynamic change in the J wave is one of the most
important characteristic ECG findings in patients
with ER syndrome. Nam et al. investigated the initiation of VF episodes and reported a dramatic but very
transient accentuation of J waves prior to the development
of electrical storm.7 In many patients affected
by ER syndrome, a spontaneous beat-to-beat fluctuation
in the morphologic pattern of the ER was observed
in addition to the spontaneous accentuation of
the J wave amplitude preceding the electrical storm.
In the present case, the patient presented with SCD
caused by VF. Coronary angiography and echocardiography
did not show any structural abnormality
responsible for the VF. ECG at HD1 showed typical
ECG findings of ER syndrome, consisting of a slurred
elevation of the J-point in the inferolateral lead.
Furthermore, VF redeveloped at HD1. On the followup
serial ECG, the amplitude of the J wave was decreased.
This case therefore represents another example
illustrating the association between a dynamic
change in the J wave and the development of VF.
References
- Moss AJ, Schwartz PJ, Crampton RS, Locati E, Carleen E. The
long QT syndrome: A prospective international study.
Circulation.
1985;71:17-21.
- Gaita F, Giustetto C, Bianchi F, Wolpert C, Schimpf R, Riccardi R,
Grossi S, Richiardi E, Borggrefe M.. Short QT syndrome: A familial
cause of sudden death.
Circulation.
2003;108:965-970.
- Brugada J, Brugada R, Brugada P. Right bundle-branch block and
ST-segment elevation in leads V1 through V3: A marker for sudden
death in patients without demonstrable structural heart disease.
Circulation.
1998;97:457-460.
- Haissaguerre M, Derval N, Sacher F, Jesel L, Deisenhofer I, de Roy L, Pasquie JL, Nogami A, Babuty D, Yli-Mayry S, De Chillou C, Scanu
P, Mabo P, Matsuo S, Probst V, Le Scouarnec S, Defaye P, Schlaepfer J,
Rostock T, Lacroix D, Lamaison D, Lavergne T, Aizawa Y, Englund A,
Anselme F, O'Neill M, Hocini M, Lim KT, Knecht S, Veenhuyzen GD,
Bordachar P, Chauvin M, Jais P, Coureau G, Chene G, Klein GJ,
Clementy J. Sudden cardiac arrest associated with early repolarization.
N Engl J Med.
2008;358:2016-2023.
- Rosso R, Kogan E, Belhassen B, Rozovski U, Scheinman MM, Zeltser D,
Halkin A, Steinvil A, Heller K, Glikson M, Katz A, Viskin S. J-point
elevation in survivors of primary ventricular fibrillation and matched control subjects: Incidence and clinical significance.
J Am Coll Cardiol.
2008;52:1231-1238.
- Tikkanen JT, Anttonen O, Junttila MJ, Aro AL, Kerola T, Rissanen
HA, Reunanen A, Huikuri HV. Long-term outcome associated
with early repolarization on electrocardiography.
N Engl J Med.
2009;361:2529-2537.
- Nam GB, Ko KH, Kim J, Park KM, Rhee KS, Choi KJ, Kim YH,
Antzelevitch C. Mode of onset of ventricular fibrillation in patients
with early repolarization pattern vs Brugada syndrome.
Eur Heart J.
2010;31:330-339.
|
|
|