|
|
International Journal of Arrhythmia 2014;15(4): 4-13.
|
 |
| ORIGINAL ARTICLE |
Electrocardiographic Features of
Therapeutic Hypothermia |
|
|
 |
 |
Introduction
Therapeutic hypothermia (TH) has emerged as an important adjunctive therapy of cardiac arrest victims recommended by the international
resuscitation guidelines.1,2 The positive effects on improvement in neurologic function and survival have been proved in two recent trials.3,4
Characteristic electrocardiographic (ECG) changes occur in patients with hypothermia. The J wave, also known as the Osborn wave, is the most
characteristic ECG feature in hypothermia.5 The J wave is also noted in certain non-hypothermic
conditions such as Brugada syndrome and early
repolarization syndromes (ERS). The presence of J
waves in such syndromes is related to the occurrence
of ventricular fibrillation (VF), leading to sudden
death. However, whether hypothermic patients with
J waves are susceptible to fatal ventricular
arrhythmia remains undetermined. Previous reports
have shown that the incidence of ventricular
arrhythmia is unexpectedly low in hypothermic
patients with J waves, varying from 0% to 2%.6-8
In the present study, we investigated
electrocardiographic changes induced by TH and the
possible arrhythmogenic potential of the
TH-induced J waves.
Methods
Study Design
During the study period from August 2010 to August 2013, 68 patients underwent TH after return
of spontaneous circulation. The patients' medical records were reviewed to evaluate clinical
characteristics such as age, sex, vital signs, cause of arrest, initial rhythm, and ECG findings on
admission. To achieve the assigned temperature as
rapidly as possible, ice-cold fluids and surface temperature-management devices (ARCTIC SUN®Temperature Management System, BARD Medical,
CO) were utilized. The following recommendations
were made: cool unconscious patients to 33℃ within
12 hours post-restoration of spontaneous circulation;
achieve the desired patient temperature as rapidly as
possible; maintain the target temperature for 24
hours; rewarm gradually to 36.5℃ in hourly
increments of 0.1-0.25℃/h; and maintain
normothermia of ~37.5℃ after rewarming. We
compared the clinical characteristics and basic ECG
parameters of patients with and without J waves.
The study protocol was reviewed and approved by
the Ethics Committee of the College of Medicine,
Ulsan University.
ECG Analysis
The following ECG parameters were analyzed:
heart rate, PR interval, duration of the QRS
complex, and QT and QTc intervals. J wave was
defined as notches or slurs in the terminal part of
the QRS complex with an amplitude ≥0.1 mV above
the isoelectric line in at least 2 contiguous leads.9
The J-wave amplitude was measured as the
difference between the top of the J wave and the
isoelectric line using Cardio Calipers (On-Screen
Electrocardiogram Measurement) from Iconico.com.
For the comparison of the distribution of J wave,
ECG lead areas were grouped as right precordial (V1-3),
left precordial (V4-6), high lateral (I, aVL), and inferior
(II, III, and aVF).
Statistical Analysis
All statistical analyses were performed with SPSS
software (SPSS Inc., Chicago, IL). Categorical variables were analyzed by the χ2 test. Continuous
variables were analyzed by the t-test. A P value <0.05 was regarded as significant.
Results
Clinical Characteristics
A total of 68 patients (mean age, 59.8±1.7 years; 42 male) who underwent TH were analyzed. The
mean body temperature on TH was 33.3±0.1℃. J
waves were observed in 40 patients during TH. J
waves were newly developed in 37 patients and
preexisting J waves were augmented in three
patients. Two patients with ERS and a patient with
alcoholic ketoacidosis displayed preexisting J waves
on 12 lead ECG prior to TH. Figure 1 displays
representative examples of J waves recorded during
TH. A patient with ERS had prominent J waves
compared to a patient with non-cardiogenic arrest.
Clinical and ECG characteristics are presented in
Table 1. There were no significant differences
between patients with and without J waves in terms
of age, sex, temperature achieved during TH and
ECG parameters.


ECG Changes Observed during TH
ECG tracings were assessed for the presence of
TH-induced electrocardiographic changes. A
consistent reduction in heart rate from 102±29 to
86±23 beats/min (15.4% reduction, p<0.0001) was
observed. QRS duration showed a significant (10.7%)
increase from 94.3±17.5 ms before TH to
104.4±25.4 ms during TH (p=0.001). The QT and
QTc intervals displayed significant 18.5% and 8.7%
increases, respectively (371.1±63.3 ms before TH to
439±86.9 ms during TH, p<0.0001, and
468.0±44.2 ms before TH to 512.7±74.6 ms during
TH, p<0.0001).
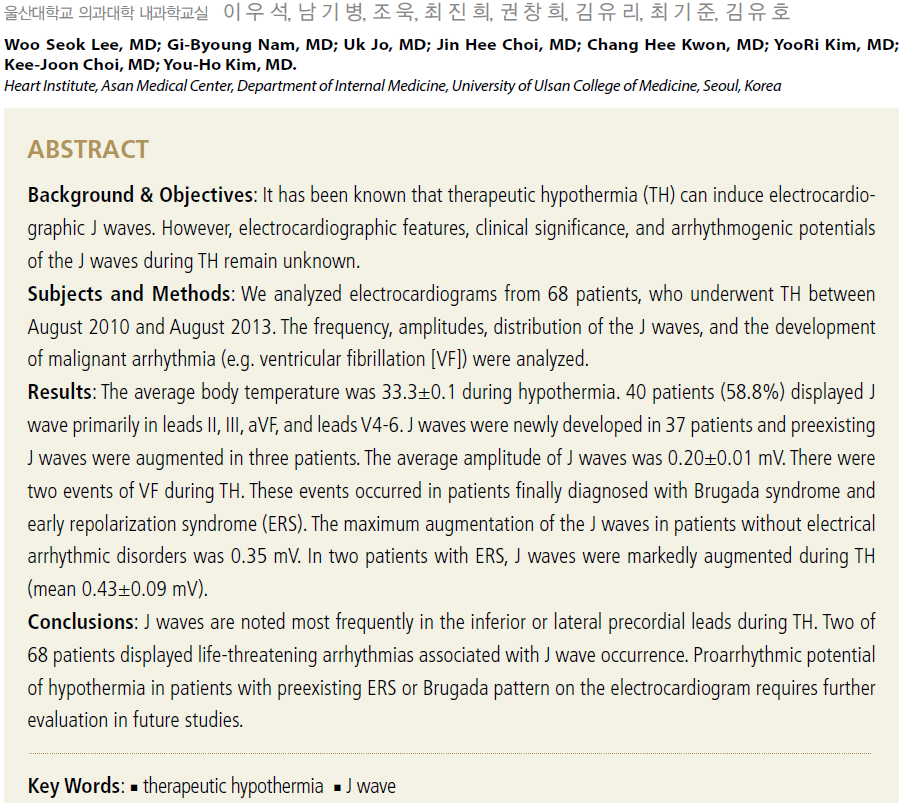
Causes of Cardiac Arrest and Initial Rhythm
The causes of cardiac arrests were highly variable.
Cardiac causes were responsible in 16.2% of the
study subjects, while non-cardiac etiology was
present in 75.0% of the patients (Table 2). In cardiac etiology, acute myocardial ischemia caused by
myocardial infarction or coronary artery spasm
predominated.
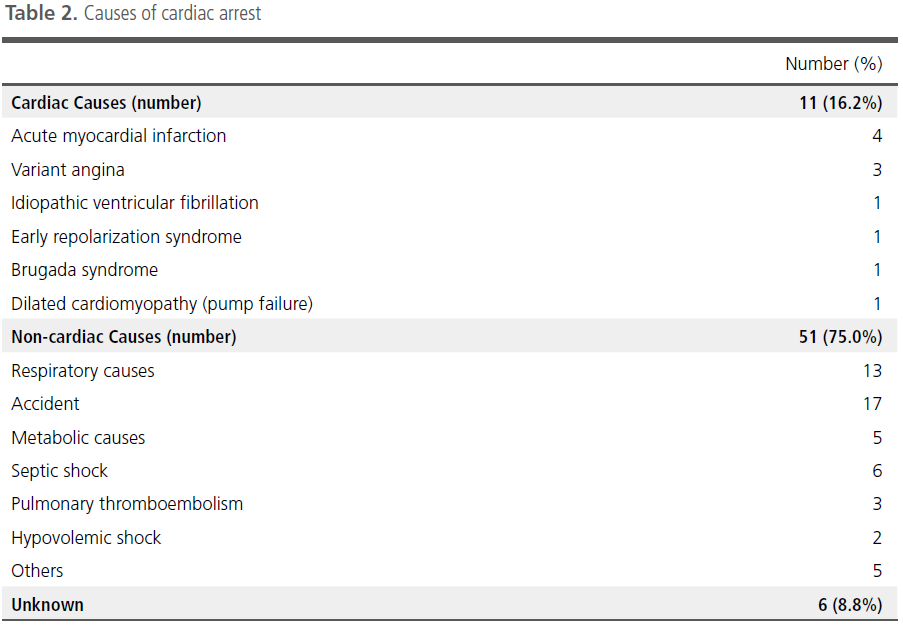
Initial rhythm determined by ECGs at the
emergency room is shown in Table 3. VF was
present in 10/11 (90.1%) of patients, and pulseless
electrical activity/asystole was recorded in 1/11 (9.1%)
of the patients in the cardiac etiology group.
However, VF was present in only 4/47 (7.8%) of the
non-cardiac cause patients.
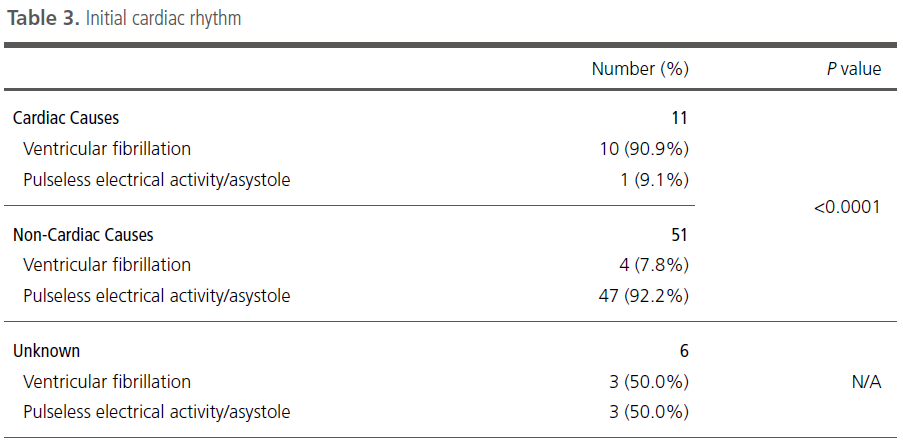
Distribution and Mean Amplitude of J Wave during TH
As shown in Table 4, J waves were common in the
inferior and left precordial leads, followed by the
high lateral and right precordial leads. Although the
frequency of J waves was low in the right precordial
leads, the mean amplitudes of J waves (when
observable) were higher in the right precordial leads
than in other ECG leads. This resulted in prominent
right precordial J wave augmentation in two patients
with primary arrhythmic disorders. In these patients, J waves were markedly augmented during
TH compared with the remainder (0.450±0.095 vs.
0.173±0.012 mV).
Patients who Developed VF during TH
VF occurred in two patients during TH. The two
patients were later diagnosed with Brugada
syndrome and ERS, respectively. A 56-year-old
male patient who was diagnosed with Brugada
syndrome displayed newly developed J wave in the
left precordial leads during TH (at 32.8℃). However,
the J-ST segment elevation in V1 and V2 became
diminished during TH. J waves in the left precordial
leads occurred immediately post DC cardioversion for
VF (Figure 2). A 70-year-old male patient, who was
diagnosed with ERS, had marked augmentation of J
wave in the left precordial leads (V3-4) during TH (at
33.2℃) (Figure 3). Prominent J waves were observed
after DC cardioversion for VF. The two patients
underwent cardioverter/defibrillator implantation
prior to discharge.


Discussion
The main findings of this study are as follows: (1)
J waves were induced or augmented in 58.8% of the
patients undergoing mild TH (target temperature
33℃); (2) J waves appeared more commonly in the
inferior and lateral leads than in the right precordial
leads; and (3) it was hypothesized that patients with
primary arrhythmic disorders displayed a higher
prevalence and amplitude of J waves and were more
vulnerable to develop VF during TH than those
without primary arrhythmic disorders.
Recent population-based studies have established
an association between the early repolarization
pattern and VF, whether idiopathic in nature or
secondary to ischemia.10-12 The tendency for
hypothermia to induce similar electrocardiographic
changes is well established.5,13 Consequently, TH post
cardiac arrest can provide an opportunity to examine
the impact of J wave-associated hypothermia on malignant arrhythmic potential.14 This retrospective
cohort study assessed the impact of TH on the
prevalence, distribution, and magnitude of J waves,
and their association with malignant arrhythmia.
During the cooling phase, 58.8% of our study
population displayed J wave above 0.1 mV. It is well
documented that the prevalence of J wave varies
with core temperature.15,16 Reports on patients with
accidental hypothermia suggest that the prevalence
of J wave would be minimal during mild
hypothermia (temperature 33℃).15-17 However,
Rolfast et al reported a 30% prevalence of J waves
during TH18 and the most recent study by Williams
et al discovered a prevalence of J wave (51.2%)
similar to our study findings.19 According to these
results and our observations, the prevalence of J
wave during TH appears higher than previously
reported.
Similar to results of previous reports, the J wave
was most frequently recorded in the leads facing the left ventricle and in the inferior limb leads.20 Recent
data show that the inferolateral J wave is
occasionally malignant and therefore strongly
associated with sudden cardiac death.10,21 In addition,
the inferolateral J wave in Brugada syndrome is
significantly associated with a poor prognosis.22-25 In
this study, VF occurred in two patients with primary
arrhythmia disorder (Brugada syndrome and ERS).
The small number of subjects in this study made it
difficult to estimate the incidence of VF during TH.
From our results alone, we cannot determine the
relationship between the presence of J waves and
the incidence of VF in the general population.
Nontheless, considering the temporal relationship
between the J wave and VF occurrence, TH may
serve as a trigger for VF in certain susceptible
patients. Incidence of VF in patients with primary
arrhythmic disorder in comparison with the general
population needs to be determined in future
prospective studies. Recently, a Target Temperature
Management trial26 showed that hypothermia, at a
targeted temperature of 33℃, did not confer a
benefit as compared with a targeted temperature of
36℃. After consideration of this finding, a targeted
temperature of 36℃ may be a safe alternative to
avoid potential TH complications while treating
abnormal patient groups (e.g., primary arrhythmia
disorder patients).
Conclusion
J waves were present in the majority of patients
undergoing TH after cardiac arrest. TH-related J
waves were most frequently recorded in the inferior
and lateral precordial leads. VF was rarely observed
(2.7%) and was confined to patients with Brugada
syndrome or ERS. Although this study cannot prove
causality between the VF and the J wave during TH,
it illustrates a temporal relationship between
hypothermia and increased frequency of malignant
arrhythmias in patients with primary arrhythmic
disorders. Application of TH may require careful
attention in this susceptible, high-risk population.
References
- Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, Gabrielli A, Silvers SM, Zaritsky AL, Merchant R, Vanden Hoek TL, Kronick SL and American Heart A. Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care.
Circulation.
2010;122:S768-786.
- Deakin CD, Nolan JP, Soar J, Sunde K, Koster RW, Smith GB and Perkins GD. European Resuscitation Council Guidelines for Resuscitation 2010 Section 4. Adult advanced life support.
Resuscitation.
2010;81:1305-1352.
- Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G and Smith K. Treatment of comatose survivors of out-ofhospital cardiac arrest with induced hypothermia.
N Engl J Med.
2002;346:557-563.
- Hypothermia after Cardiac Arrest Study G. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest.
N Engl J Med.
2002;346:549-556.
- Osborn JJ. Experimental hypothermia; respiratory and blood pH changes in relation to cardiac function.
Am J Physiol.
1953;175:389-398.
- Delaney KA, Vassallo SU, Larkin GL and Goldfrank LR. Rewarming rates in urban patients with hypothermia: prediction of underlying infection.
Acad Emerg Med.
2006;13:913-921.
- Rankin AC and Rae AP. Cardiac arrhythmias during rewarming of patients with accidental hypothermia.
Br Med J (Clin Res Ed).
1984;289:874-877.
- Vassal T, Benoit-Gonin B, Carrat F, Guidet B, Maury E and Offenstadt G. Severe accidental hypothermia treated in an ICU: prognosis and outcome.
Chest.
2001;120:1998-2003.
- Antzelevitch C. Genetic, molecular and cellular mechanisms underlying the J wave syndromes.
Circ J.
2012;76:1054-1065.
- Haissaguerre M, Derval N, Sacher F, Jesel L, Deisenhofer I, de Roy L, Pasquie JL, Nogami A, Babuty D, Yli-Mayry S, De Chillou C, Scanu P, Mabo P, Matsuo S, Probst V, Le Scouarnec S, Defaye P, Schlaepfer J, Rostock T, Lacroix D, Lamaison D, Lavergne T, Aizawa Y, Englund A, Anselme F, O'Neill M, Hocini M, Lim KT, Knecht S, Veenhuyzen GD, Bordachar P, Chauvin M, Jais P, Coureau G, Chene G, Klein GJ and Clementy J. Sudden cardiac arrest associated with early repolarization.
N Engl J Med.
2008;358:2016-2023.
- Patel RB, Ng J, Reddy V, Chokshi M, Parikh K, Subacius H, Alsheikh-Ali AA, Nguyen T, Link MS, Goldberger JJ, Ilkhanoff L and Kadish AH. Early repolarization associated with ventricular arrhythmias in patients with chronic coronary artery disease.
Circ Arrhythm Electrophysiol.
2010;3:489-495.
- Rosso R, Kogan E, Belhassen B, Rozovski U, Scheinman MM, Zeltser D, Halkin A, Steinvil A, Heller K, Glikson M, Katz A and Viskin S. J-point elevation in survivors of primary ventricular fibrillation and matched control subjects: incidence and clinical significance.
J Am Coll Cardiol.
2008;52:1231-1238.
- Emslie-Smith D, Sladden GE and Stirling GR. The significance of changes in the electrocardiogram in hypothermia.
Br Heart J.
1959;21:343-351.
- Bastiaenen R, Hedley PL, Christiansen M and Behr ER. Therapeutic hypothermia and ventricular fibrillation storm in early repolarization syndrome.
Heart rhythm.
2010;7:832-834.
- Vassallo SU, Delaney KA, Hoffman RS, Slater W and Goldfrank LR. A prospective evaluation of the electrocardiographic manifestations of hypothermia.
Acad Emerg Med.
1999;6:1121-1126.
- Higuchi S, Takahashi T, Kabeya Y, Hasegawa T, Nakagawa S and Mitamura H. J waves in accidental hypothermia.
Circ J.
2013;78:128-134.
- Mattu A, Brady WJ and Perron AD. Electrocardiographic manifestations of hypothermia.
Am J Emerg Med.
2002;20:314-326.
- Rolfast CL, Lust EJ and de Cock CC. Electrocardiographic changes in therapeutic hypothermia.
Crit Care.
2012;16:R100.
- Williams SE, Sabir I, Nimmo C, Linton N, Sebag FA, Harrison JL, Wright M, Barrett NA, Shankar-Hari M and O'Neill MD. Quantitative assessment of the effects of therapeutic hypothermia on early repolarization in idiopathic ventricular fibrillation survivors: a 7-year cohort study.
Circ Arrhythm Electrophysiol.
2014;7:120-126.
- Gussak I, Bjerregaard P, Egan TM and Chaitman BR. ECG phenomenon called the J wave. History, pathophysiology, and clinical significance.
J Electrocardiol.
1995;28:49-58.
- Haissaguerre M, Sacher F, Nogami A, Komiya N, Bernard A, Probst V, Yli-Mayry S, Defaye P, Aizawa Y, Frank R, Mantovan R, Cappato R, Wolpert C, Leenhardt A, de Roy L, Heidbuchel H, Deisenhofer I, Arentz T, Pasquie JL, Weerasooriya R, Hocini M, Jais P, Derval N, Bordachar P and Clementy J. Characteristics of recurrent ventricular fibrillation associated with inferolateral early repolarization role of drug therapy.
J Am Coll Cardiol.
2009;53:612-619.
- Kamakura S, Ohe T, Nakazawa K, Aizawa Y, Shimizu A, Horie M, Ogawa S, Okumura K, Tsuchihashi K, Sugi K, Makita N, Hagiwara N, Inoue H, Atarashi H, Aihara N, Shimizu W, Kurita T, Suyama K, Noda T, Satomi K, Okamura H, Tomoike H and Brugada Syndrome Investigators in J. Long-term prognosis of probands with Brugada-pattern ST-elevation in leads V1-V3.
Circ Arrhythm Electrophysiol.
2009;2:495-503.
- Kawata H, Morita H, Yamada Y, Noda T, Satomi K, Aiba T, Isobe M, Nagase S, Nakamura K, Fukushima Kusano K, Ito H, Kamakura S and Shimizu W. Prognostic significance of early repolarization in inferolateral leads in Brugada patients with documented ventricular fibrillation: a novel risk factor for Brugada syndrome with ventricular fibrillation.
Heart rhythm.
2013;10:1161-1168.
- Sarkozy A, Chierchia GB, Paparella G, Boussy T, De Asmundis C, Roos M, Henkens S, Kaufman L, Buyl R, Brugada R, Brugada J and Brugada P. Inferior and lateral electrocardiographic repolarization abnormalities in Brugada syndrome.
Circ Arrhythm Electrophysiol.
2009;2:154-161.
- Takagi M, Aonuma K, Sekiguchi Y, Yokoyama Y, Aihara N, Hiraoka M and Japan Idiopathic Ventricular Fibrillation Study I. The prognostic value of early repolarization (J wave) and ST-segment morphology after J wave in Brugada syndrome: multicenter study in Japan.
Heart rhythm.
2013;10:533-539.
- Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, Horn J, Hovdenes J, Kjaergaard J, Kuiper M, Pellis T, Stammet P, Wanscher M, Wise MP, Aneman A, Al-Subaie N, Boesgaard S, Bro-Jeppesen J, Brunetti I, Bugge JF, Hingston CD, Juffermans NP, Koopmans M, Kober L, Langorgen J, Lilja G, Moller JE, Rundgren M, Rylander C, Smid O, Werer C, Winkel P, Friberg H and Investigators TTMT. Targeted temperature management at 33 degrees C versus 36 degrees C after cardiac arrest.
N Engl J Med.
2013;369:2197-2206.
|
|
|
|