|
|
International Journal of Arrhythmia 2014;15(4): 37-44.
|
 |
| ECG & EP CASES |
Atrial Tachycardia in a Patient with
Extracardiac Conduit Fontan Circulation |
|
 |
 |

Introduction
The survival rate of patients with complex congenital
heart disease has recently improved, most
likely due to the development of new surgical
techniques and improved perioperative medical
management.1 As the number of adult patients
with congenital heart disease has increased, arrhythmias
and heart failure are becoming growing
issues in these patients.1 Thus, it is not surprising
that the demand for electrophysiologic
(EP) studies and radiofrequency catheter ablation
(RFCA) is increasing. EP studies and RFCA
are challenging in patients who have undergone
extracardiac conduit Fontan procedures for the
palliative treatment of congenital heart disease,
because the systemic venous blood is not drained
into the heart in these techniques. Here, we report
a case of focal atrial tachycardia, which was
ablated via a trans-conduit puncture in a patient
who had undergone an extracardiac conduit Fontan
procedure.
Case
A 14-year-old male patient visited the emergency
room complaining of palpitations for 3 hours. He had experienced several episodes of
palpitations during the past year. His blood pressure
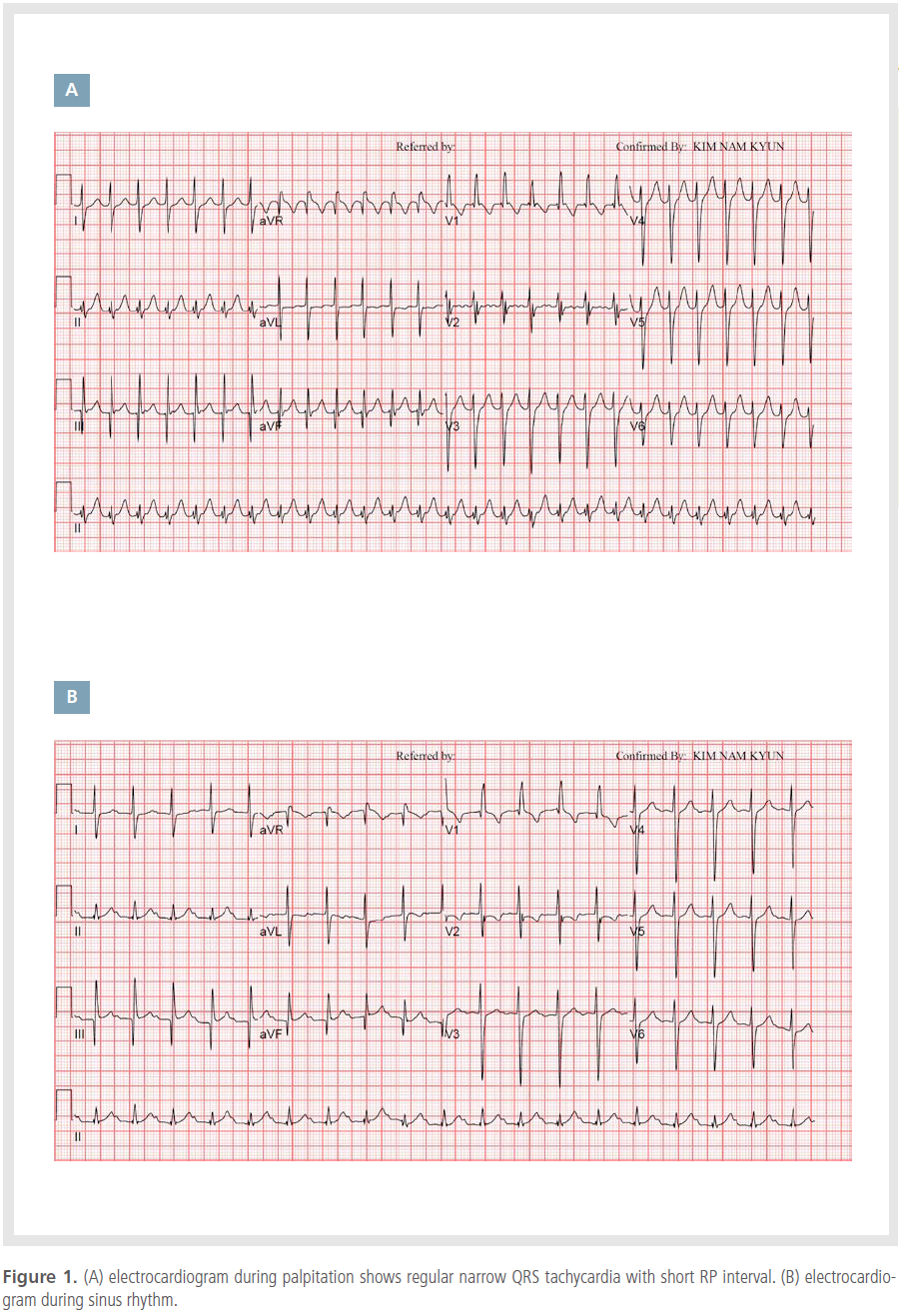
was 82/49 mmHg. The electrocardiogram
(ECG) showed regular, narrow QRS tachycardia
with a rate of 160 beats/min and a short RP interval
(Figure 1A). In the emergency room, the
tachycardia spontaneously converted into sinus
rhythm (Figure 1B). The QRS morphology of the
tachycardia was similar to that in sinus rhythm.
When he was 10 days old, he was diagnosed
with double-inlet left ventricle (DILV), complete
transposition of the great arteries (TGA), and
large ventricular septal defect (VSD). When he
was 5 months old, the bidirectional cavopulmonary
shunt and interatrial septectomy were performed
for palliation. At the age of 1 year, an
extracardiac conduit Fontan procedure was performed
with the autologous pericardium. We decided
to perform the EP study for diagnosis and
treatment of the tachycardia. Cardiac computed
tomography (CT) was performed for assessment
of the heart anatomy, showing findings compatible
with TGA, DILV, large VSD, functional single
ventricle, and extracardiac Fontan conduit (Figure 2).


Both femoral veins were punctured. Conduit
angiography was performed with a Bermantype
angiography catheter (Arrow International,
Reading, PA, USA) (Figure 3A). Two SR-0 Swartz
transseptal introducer sheath (St Jude Medical, St
Paul, MN, USA), a snare catheter (PFM Medical,
Nonnweiler, Germany), and an intracardiac
echocardiography catheter (AcuNav, Siemens,
Mountain View, CA, USA) were inserted into the
Fontan conduit via the femoral veins. A BRK-1
Brockenbrough transseptal needle (St Jude Medical)
was inserted into the Swartz sheath, and the
dilator tip of the Swartz sheath was held with the
snare catheter to prevent it from sliding up along
the conduit wall (Figure 3B and D). We punctured
the wall between the conduit and the right atrium
with the Brockenbrough transseptal needle under
intracardiac echocardiography guidance (Figure
3C). Right and left atriography was performed
with the pigtail catheter via the trans-conduit
puncture. A deflectable decapolar catheter (St Jude Medical) was placed in the high left atrium
via the Swartz sheath and a decapolar catheter
(St Jude Medical) was placed in the ventricle via
the aorta (Figure 4A). The initial rhythm was
normal sinus rhythm. During ventricular pacing
and single ventricular extrastimuli, the atrial
electrogram showed one-to-one ventriculoatrial
conduction with decremental properties. During
the atrial pacing of 240 ms and infusion of isoproterenol
at a rate of 2 μg/min, tachycardia with
a 290 ms cycle length was induced. Tachycardia
was maintained despite the presence of a premature
ventricular complex and atrioventricular
block (Figure 5A and B). Therefore, atrioventricular
reentrant tachycardia could be excluded.
During tachycardia, the atrioventricular or ventriculoatrial
interval varied (Figure 5B). It was not
compatible with atrioventricular nodal reentrant
tachycardia. The tachycardia was not entrainable
by ventricular pacing. The decapolar catheter was
moved to the right atrium (RA) side in the Fontan conduit, and an irrigated ablation catheter (Thermocool,
Biosense Webster, Diamond Bar, CA,
USA) was inserted into the atrium via the conduit
puncture for tachycardia mapping (Figure
4B). During tachycardia, 3-dimensional electroanatomical
mapping was performed with CARTO
(Biosense Webster, Diamond Bar, CA, USA). The
tachycardia was originating from the mid portion
of the remnant interatrial septum (Figure 6).
The tachycardia was compatible with focal atrial
tachycardia originating from the interatrial septum.
During sinus rhythm, we mapped the His
bundle potentials. The His bundle area was located
in the lower posterior potion of the interatrial
septum. The origin of the tachycardia was away
from the His bundle area by 13.6 mm (Figure 6B).
We performed RFCA of the origin of the atrial
tachycardia by delivering 30 watts of RF energy
for 90 s with the irrigated ablation catheter during
sinus rhythm. The procedure ended after we
confirmed that the tachycardia was not induced by the programmed electric stimulation and isoproterenol
infusion. The patient had no symptom
and maintained sinus rhythm for 6 months after
RFCA.


Discussion
The case was focal atrial tachycardia originating
from the septum in a patient who had undergone
an extracardiac conduit Fontan procedure.
We performed an EP study and RFCA of the origin
of the focal atrial tachycardia successfully via
the trans-conduit puncture.
The lifelong prevalence of atrial tachycardia
in patients with extracardiac Fontan circulation
is approximately 50%,2-4 and it is considerably
higher than in the normal population. In patients
with extracardiac conduit Fontan circulation, it
is difficult to perform an EP study, because the
heart is completely excluded from the systemic
venous system. There were previous case reports
of EP studies and RFCA via various routes
in patients with Fontan circulation, including
via a trans-thoracic puncture, sternotomy approach,
trans-apical access and trans-conduit
puncture.5-8
The EP catheters can be transvascularly
placed via 2 pathways: the trans-conduit
puncture and retrograde transaortic approach.
The approach via the trans-conduit puncture is
suitable for gaining access to the atrium and the
retrograde transaortic approach is suitable for
gaining access to the ventricle. It is challenging
to puncture the Fontan conduit because fibrosis
forms around the conduit. In addition, the conduit
wall is vertical-unlike the interatrial septum-
and the transseptal needle tends to slide up
along the conduit wall instead of puncturing it.
The use of a Brockenbrough transseptal needle
while holding the dilator tip of the Swartz sheath
with a snare catheter is a useful method for puncturing the Fontan conduit.9 A large-curve
BRK-1 transseptal needle is superior to a smallcurve
BRK needle. Moreover, the radiofrequency
transseptal needle can be a good option for puncturing
the fibrotic Fontan conduit.
In patients with congenital heart disease, the
EP study and RFCA are very challenging because
of the unusual anatomy of the heart. In addition,
it is common for patients to have vascular anomalies
including a persistent left superior vena cava
and inferior vena cava interruption. It is important
that the operator be completely aware of the
anatomy of heart and vessels of each patient.
Every patient has a unique heart structure, even
though this patient group has the same diagnosis
of congenital heart disease. The operator needs
to review and understand the previous cardiac
surgery and intervention. The operator should
make a meticulous plan for the procedure, taking
into consideration the types of EP catheters to be
used for each chamber, pathways to be used for
positioning of the EP catheters, and appropriate
angles for the X-ray beam to improve visualization.
The operator needs to discuss the current
hemodynamics and long-term prognosis of the
patient with the pediatric cardiologists. Given the
complex heart anatomy, cardiac CT and a 3-dimensional
electroanatomic mapping system are
necessary for guiding the procedure. Intracardiac
echocardiography can be helpful for real-time
visualization of the anatomy and EP catheters.
The activated coagulation time should be maintained
at 350-400 ms by heparin infusion during
the EP study in patients with a single ventricle,
as the catheters are placed in the systemic chambers.
In the present case, the remnant interatrial
septum might become arrhythmogenic after septectomy
due to degenerative changes of the interatrial
septum. This patient is likely to develop atrial tachyarrhythmia originating from other
parts of the atrium. In addition, an advanced
atrioventricular block can occur in the future,
although the peri-procedural ECG showed first
degree atrioventricular block. Thus, the patient
will require long-term follow-up.
Conclusion
EP studies and RFCA are feasible via a transconduit
puncture in patients with extracardiac
conduit Fontan circulation.
References
- Mackie AS, Ionescu-Ittu R, Therrien J, Pilote L, Abrahamowicz M, Marelli AJ. Children and adults with congenital heart disease lost to follow-up; who and when?
Circulation. 2009;120:302-309.
- Gelatt M, Hamilton RM, McCrindle BW, Gow RM, Williams WG, Trusler GA, Freedom RM. Risk factors for atrial tachyarrhythmias after the Fontal operation.
J Am Coll Cardiol. 1994;24:1735-1741.
- Weipert J, Noebauer C, Schreiber C, Kostolny M, Zrenner B, Wacker A, Hess J, Lange R. Occurrence and management of atrial arrhythmia after long-term Fontan circulation.
J Thorac Cardiovasc Surg. 2004;127:457-464.
- Lasa JJ, Glatz AC, Daga A, Shah M: Prevalence of arrhythmias late after the Fontan operation.
Am J Cardiol. 2014;133:1184-1188.
- Nehgme R, Carboni MP, Care J, Murphy JD. Transthoracic percutaneous access for electroanatomic mapping and catheter ablation of atrial tachycardia in patients with a lateral tunnel Fontan.
Heart Rhythm. 2006;3:37-43.
- Khairy P, Fournier A, Ruest P, Vobecky SJ. Transcatheter ablation via a sternotomy approach as a hybrid procedure in a univentricular heart.
Pacing Clin Electrophysiol. 2008;31:639-640.
- Brown SC, Boshoff DE, Rega F, Eyskens B, Budts W, Heidbuechel H, Meyns B, Gewillig M. Transapical left ventricular access for difficult to reach interventional targets in the left heart.
Catheter Cardiovasc Interv. 2009;74:137-142.
- Dave AS, Aboulhosn J, Child JS, Shivkumar K. Transconduit puncture for catheter ablation of atrial tachycardia in a patient with extracardiac Fontan palliation.
Heart Rhythm. 2010;7:413-416.
- Aoki H, Nakamura Y, Takeno S, Takemura T. A new procedure for a transconduit puncture by grasping the dilator tip with a snare catheter: an alternative access method during catheter ablation of supraventricular tachycardias after an extracardiac Fontan operation.
Heart Rhythm. 2014;11:1492-1494.
|
|
|
|