|
|
International Journal of Arrhythmia 2014;15(4): 49-53.
|
 |
| ECG & EP CASES |
Successful Use of a New Oral
Anti-coagulant in a Stroke Patient
with Poor Prothrombin Time Control
Even After Warfarin Treatment |

|
|
 |
 |

Introduction
For the last several decades, vitamin K antagonists
(VKAs) have been the primary medication
in anti-coagulant therapy for the prevention
and treatment of thrombotic events. Due to
the individual variation in prothrombin time (PT)
responses, individualized adjustment of the VKA
dose is essential to manage the international
normalized ratio (INR); however, this places a
significant practical burden on both the physician
and patient. Appropriate INR management
is very difficult in some cases, which makes
the application of therapy involving fixed doses
of oral anti-coagulants an attractive option
for practical reasons. New oral anti-coagulants
(NOACs) have recently been developed to prevent
embolic stroke and to reduce the incidence
of major bleeding in comparison with that associated
with VKA use.1,2 In the present report,
the author presents a case with poor INR control
with warfarin treatment that was successfully
treated with a NOAC to prevent embolic stroke
recurrence.

Case
A 76-year-old woman was referred to our institution
in June 2010 for the evaluation of newly
diagnosed atrial fibrillation that occurred 3 days
after an episode of transient right-side motor
weakness. She had been diagnosed with essential
hypertension 15 years previously and was taking
losartan (50 mg q.d.) and hydrochlorothiazide
(12.5 mg q.d.). Her body temperature was
36.7°C, her pulse rate was 78 beats per minute,
and her blood pressure was 126/78 mmHg. Her
radial pulse was irregular, and a grade III systolic
murmur could be heard in her mitral valve area. She showed no neurologic deficit and was mentally
alert.

 As previously stated, the patient had experienced
transient right-side motor weakness (for
approximately 2 hours) 3 days previously and had
been admitted to undergo evaluation of newly
diagnosed paroxysmal atrial fibrillation. Her
hemogram values, biochemical marker levels,
and thyroid hormone levels were within normal
limits. The initial electrocardiogram (ECG) confirmed
the presence of atrial fibrillation (Figure
1). Transthoracic echocardiography showed normal
left ventricular systolic function (ejection
fraction, 58%) and grade II mitral regurgitation.
The left atrium was mildly enlarged (diameter,
42.4 mm). Because the anterolateral ECG leads
showed ST segment depression (Figure 1), she
underwent a coronary angiogram, which indicated
a fixed atherosclerotic lesion in the middle
segment of the left anterior descending artery
and showed 70% stenosis (Figure 2). Percutaneous
coronary intervention was not performed as
she did not experience any chest pain or discomfort.
Therefore, the author decided to use a class
Ic anti-arrhythmic drug (flecainide) and warfarin
to prevent embolic stroke, based on her CHADS2
score of 4 (1 point for hypertension, 1 point for
age ≥75 years, and 2 points for history of transient
ischemic attack).
As previously stated, the patient had experienced
transient right-side motor weakness (for
approximately 2 hours) 3 days previously and had
been admitted to undergo evaluation of newly
diagnosed paroxysmal atrial fibrillation. Her
hemogram values, biochemical marker levels,
and thyroid hormone levels were within normal
limits. The initial electrocardiogram (ECG) confirmed
the presence of atrial fibrillation (Figure
1). Transthoracic echocardiography showed normal
left ventricular systolic function (ejection
fraction, 58%) and grade II mitral regurgitation.
The left atrium was mildly enlarged (diameter,
42.4 mm). Because the anterolateral ECG leads
showed ST segment depression (Figure 1), she
underwent a coronary angiogram, which indicated
a fixed atherosclerotic lesion in the middle
segment of the left anterior descending artery
and showed 70% stenosis (Figure 2). Percutaneous
coronary intervention was not performed as
she did not experience any chest pain or discomfort.
Therefore, the author decided to use a class
Ic anti-arrhythmic drug (flecainide) and warfarin
to prevent embolic stroke, based on her CHADS2
score of 4 (1 point for hypertension, 1 point for
age ≥75 years, and 2 points for history of transient
ischemic attack).
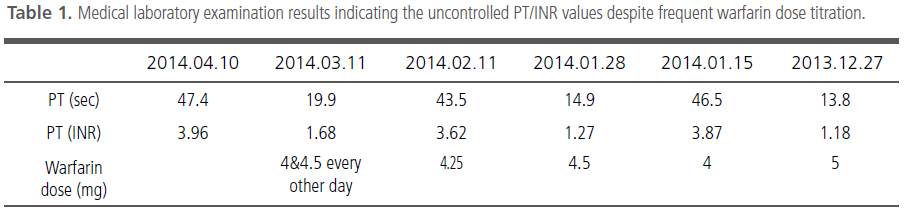
However, despite the frequent blood sampling
and visits to the outpatient clinic (which the patient complained about), her INR could not be
controlled during the follow-up period. After 3
months, her ECG showed normal sinus rhythm
(Figure 3), after which she refused to take warfarin
regardless of our recommendations. Hence,
she was treated with a combination of two anti-
coagulants (aspirin and clopidogrel). After 3
months, she presented to our emergency clinic
with right-side motor weakness and slurred
speech. Diffusion magnetic resonance images
(MRI) showed acute left middle and posterior
cerebral artery infarction (Figure 4). Following
recovery, the author recommended that the
patient should continue treatment with warfarin
to prevent embolic stroke. She accepted our
recommendation at that time and continued with
warfarin treatment after discharge. However,
despite several warfarin dose titrations, her PT/
INR control was found to be poor at every visit to
the clinic (Table 1). Moreover, when the INR increased
to above 3.5, she complained about gum
bleeding. As the INR was consistently outside the
target range of 2.5-3.5, the author decided to
switch the treatment from warfarin to a NOAC.
At present, the patient has not experienced
embolic stroke or any major or minor bleeding
events. In addition, she reported that she is satisfied
with the convenience of the new regimen.
Discussion
NOACs have been introduced worldwide to improve
anti-coagulation therapy. In patients who
show poor PT/INR control with warfarin, NOACs
may provide a particularly promising alternative.
Unlike warfarin, which has a narrow therapeutic
window and requires individualized dosing based
on the INR, NOACs have a wide therapeutic window,
thereby facilitating fixed dosing without the
need for laboratory monitoring or dose titration.
Several clinical studies on NOACs are currently
investigating protocols for dose adjustment,
managing bleeding events, and other such factors.
However, only a few studies have described
patient adherence to NOACs. Hence, the author
believes that more sustainable methods for improving
patient adherence to NOACs are needed.
Patients may be more motivated to take antihypertensive
medication if they perceive a tangible
benefit such as reduction of headache or
reduced chest flutters. However, in the absence
of such benefits, the adherence may drop-in
particular, this phenomenon may be observed in
patients undergoing warfarin treatment (most
users are chronic atrial fibrillation patients), even
though they regularly undergo inconvenient dose
monitoring.
Although NOACs are currently being prescribed
worldwide, it is uncertain whether accurate
data on complications are being reported. Major
bleeding complications have been noted with
NOAC use; however, it is not possible to make
definitive conclusions due to the lack of data on
comparisons with VKA use under real-world conditions. Patients in clinical trials of NOACs
are generally highly motivated to comply with the
requirement for regular visits and follow-up calls
and provided education regarding their disease
state and the importance of medication adherence
(monitored via pill counts).3 However, given
the lack of a requirement for regular coagulation
monitoring, this may not be observed for some
patients who are prescribed NOACs in the realworld
setting.4 This is especially critical in chronic
atrial fibrillation patients, most of whom have not
experienced a thrombotic event. The requirement
for INR monitoring in patients receiving warfarin
treatment effectively enables the monitoring of
adherence. Furthermore, the twice-daily dosing
schedules of some NOACs may be more difficult
for some patients to adhere to as compared to a
daily regimen. At present, in South Korea, the
markedly higher costs of NOACs should also be
carefully considered. Even for patients with insurance
that covers NOACs, physicians should
ascertain how much the patients pay for the
treatment with NOACs compared with warfarin.
High drug costs may result in reduced medication
adherence.
In the present case, the patient wished to discontinue
blood sampling and complained of minor
bleeding (gum bleeding). She requested to receive
NOAC treatment, regardless of the cost, and has
adhered to her medication thus far. Thus, the
author recommends that NOACs should be considered
for selected patients who wish to avoid
the limitations associated with conventional VKA
treatment.
References
- Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener HC, Joyner CD, Wallentin L, Committee R-LS, Investigators. Dabigatran versus warfarin in patients with atrial fibrillation.
N Engl J Med. 2009;361:1139-1151.
- Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, Al-Khalidi HR, Ansell J, Atar D, Avezum A, Bahit MC, Diaz R, Easton JD, Ezekowitz JA, Flaker G, Garcia D, Geraldes M, Gersh BJ, Golitsyn S, Goto S, Hermosillo AG, Hohnloser SH, Horowitz J, Mohan P, Jansky P, Lewis BS, Lopez-Sendon JL, Pais P, Parkhomenko A, Verheugt FW, Zhu J, Wallentin L, Committees A, Investigators. Apixaban versus warfarin in patients with atrial fibrillation.
N Engl J Med. 2011;365:981-992.
- Bauer KA. Pros and cons of new oral anticoagulants.
Hematology Am Soc Hematol Educ Program. 2013;2013:464-470.
- Rodriguez RA, Carrier M, Wells PS. Non-adherence to new oral anticoagulants: A reason for concern during long-term anticoagulation?
J Thromb Haemost. 2013;11:390-394.
|
|
|
|