|
Case
A 48-year old woman with dizziness and
palpitations since four months was referred to the
arrhythmia service of our hospital. She underwent
mitral valve replacement surgery with a mechanical
valve in 1998 and tricuspid valve replacement
(TVR) due to severe tricuspid regurgitation in 2007.
Operation procedures were leaflet preserving TVR,
modified Cox maze III procedure with cryoablation,
internal obliteration of the left atrial appendage, and
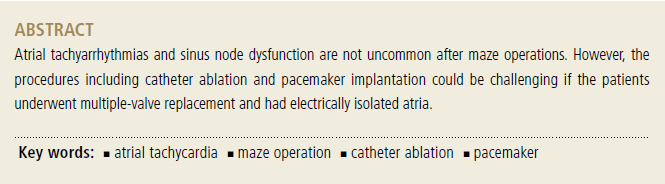
left atrial reduction plasty. ECG and Holter
recordings revealed that most of the patient’s
rhythm was atrial tachycardia (AT) with 1:1, 2:1 or
4:1 conduction and her dizziness was associated
with occasional sinus arrest following AT
termination (Figure 1). AT was resistant to a full
doses of amiodarone, thus we decided to perform
catheter ablation as well as a pacemaker implantation.
AT was macroreentrant tachycardia with a
clockwise rotation around the mitral valve annulus.
The ablation line was created in the posterolateral
mitral isthmus between the left pulmonary vein-side
maze operation line and the mitral valve annulus
(Figures 2A and 2B). AT was terminated during
ablation (Figure 2C) and a bidirectional conduction
block was confirmed. After termination of AT, the
patient’s rhythm was junctional with a heart rate of
less than 30 bpm, although the sinus node activation
was observed. The right atrium was electrically
isolated, probably due to maze operation lines and
multiple atrial scars. Pacing in the right atrium was
impossible and stimulation at the peri-mitral area of
the left atrium, including the coronary sinus, only
could pace the heart (Figure 3). Permanent
pacemaker implantation was performed after
ablation. Atrial lead placement was not considered
due to the inability of pacing in the right atrium.
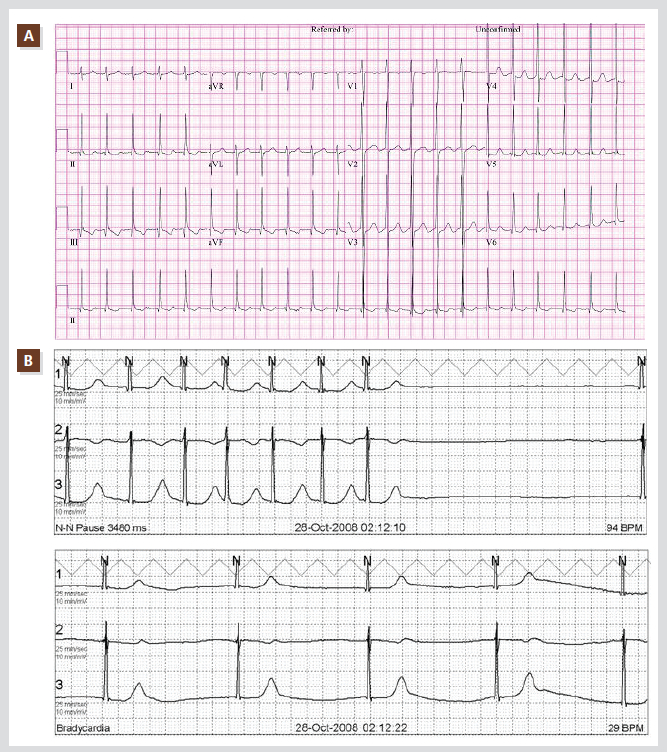
Figure 1. ECG and Holter recording. ECG obtained during atrial tachycardia with 2:1 conduction (A). Holter recording
showed termination of atrial tachycardia followed by long sinus arrest and junctional escape rhythm with 29 bpm (B).
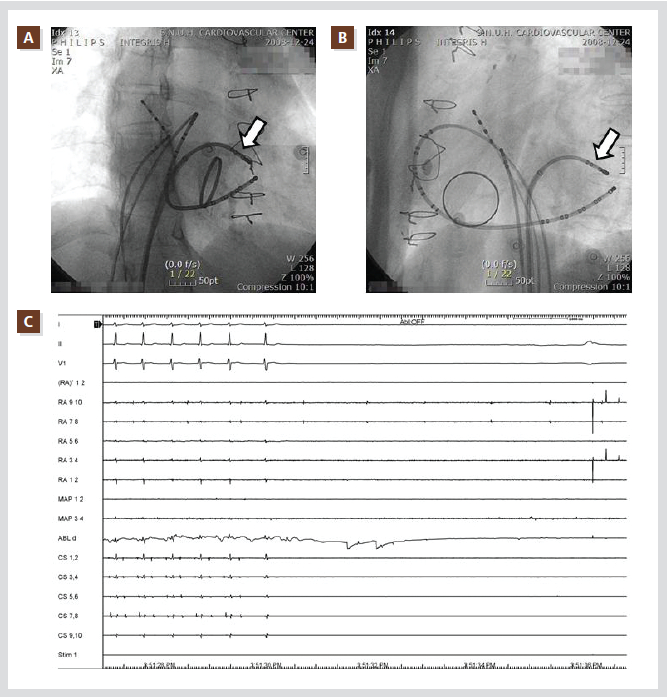
Figure 2. Ablation of atrial tachycardia. RAO (A) and LAO (B) fluoroscopic images during creation of postero-lateral
mitral isthmus line. Atrial tachycardia was terminated during ablation and long sinus arrest was observed.
Open arrows indicate the ablation catheter (C).

Figure 3. Atrial pacing after ablation heart. left atrial pacing using the coronary sinus catheter with 600 ms of cycle
length could be captured and pace the heart (A). Pacing using the electrode catheter placed in the right atrium could
not be captured. The electrograms show capture failure of the right atrium with 550 ms of stimulation during left atrial
pacing with 600 ms (B).
Ventricular lead was inserted into the great cardiac
vein due to post-TVR status (Figure 4) during
coronary sinus pacing backup because of marked
bradycardia (15~20 bpm). After catheter ablation
and pacemaker implantation, the patient did not
complain of any palpitation or dizziness during the
two-year follow-up period.
Discussion
Both atrial tachycardia/flutter and sinus node
dysfunction are relatively common in patients after
the maze operation. Atrial tachyarrhythmias
occurred in 43% of the patients.1 Among them, 41%
cases had atrial flutter with/without atrial
fibrillation. When we consider the fact that the
incidence of atypical atrial flutter after atrial
fibrillation ablation is known to be 30~50%,2 then
the number of cases after the maze operation seems
to be lower. This would be related to the completeness of lines for the conduction block.

Figure 4. Pacemaker implanted state. Chest X-rays after pacemaker implantation (A,B). ECG shows a well-functioning
pacemaker (C).
Observation without pacemaker implantation may
be possible in some patients after catheter ablation if
their bradycardias are always associated with atrial
tachycardia and if they have a relatively good sinus
node function. To determine an appropriate
management plan, ECG with normal range of heart
rate should be carefully examined in these patients
because the rhythm may not be sinus rhythm but
atrial tachycardia with a relatively slow ventricular
response (eg. 4:1 conduction) and the P waves
might be very small and have a different
morphology.3
Permanent pacemaker needs in patients that
underwent maze operations are known to be
3.9~5.8% in meta-analysis reports4,5 and slightly
higher in classical cut-and-sew Cox maze III than in
modified maze procedure using RF, microwave or
cryoenergy.4 According to the report from Dr. Cox’s
institution, the incidence of pacemaker implantation after the original Cox maze III was 9/112 (8.0%)
and 20/86 (23.3%) in lone maze and concomitant
(eg. 39 cases of mitral valve surgery and 33 cases of
coronary bypass surgery) maze procedures,
respectively.6 In the cases with pacemaker
implantation after concomitant maze procedures,
9/20 patients (45%) had preoperative diagnosis of
sick sinus syndrome. Therefore, 55% of the patients
had newly-developed sinus node dysfunction
requiring a pacemaker after the maze operation.
The incidence of atrial tachycardia/flutter and sinus
node dysfunction are common as described above
and TVR is also concomitantly performed in some
patients. Therefore, patients requiring the left
ventricular lead may be not so rare. Continuous
pacing during the procedure would be essential in
some patients with marked bradycardia like in the
present case. However, the electrode catheter placed
in the coronary sinus could not be removed when
there are no other suitable pacing sites in the right
atrium. Therefore the present case was challenging
with regards to inserting the cardiac-vein lead
during coronary sinus pacing and keeping the
position of the inserted cardiac-vein lead during the
sheath and coronary-sinus electrode catheter
removal. The other optional method for pacing
during the procedure could be left atrial pacing via
trans-septal puncture. However the stability of the
pacing catheter might be weaker than the coronary
sinus catheter. Catheter ablation could be considered
after pacemaker implantation. In that case,
manipulation of the mapping and ablation catheters
and the coronary sinus catheter placement should be
also very carefully performed to avoid dislocation of
the cardiac vein lead.
References
- Ishii Y, Gleva MJ, Gamache MC, Schuessler RB, Boineau JP, Bailey MS, Damiano RJ, Jr. Atrial tachyarrhythmias after the maze procedure: Incidence and prognosis. Circulation. 2004;110:II164- 168.
- Morady F, Oral H, Chugh A. Diagnosis and ablation of atypical atrial tachycardia and flutter complicating atrial fibrillation ablation. Heart Rhythm. 2009;6:S29-32.
- Park HE, Kim KH, Kim KB, Ahn H, Choi YS, Oh S. Characteristics of p wave in patients with sinus rhythm after maze operation. J Korean Med Sci. 2010;25:712-715.
- Khargi K, Hutten BA, Lemke B, Deneke T. Surgical treatment of atrial fibrillation; a systematic review. Eur J Cardiothorac Surg. 2005;27:258-265.
- Reston JT, Shuhaiber JH. Meta-analysis of clinical outcomes of maze-related surgical procedures for medically refractory atrial fibrillation. Eur J Cardiothorac Surg. 2005;28:724-730.
- Prasad SM, Maniar HS, Camillo CJ, Schuessler RB, Boineau JP, Sundt TM, 3rd, Cox JL, Damiano RJ, Jr. The cox maze iii procedure for atrial fibrillation: Long-term efficacy in patients undergoing lone versus concomitant procedures. J Thorac Cardiovasc Surg. 2003;126:1822-1828.
|