Bradyarrhythmia Can Increase the Plasma Level of N-Terminal Pro-Brain Natriuretic Peptide
Article information
Abstract
Background and Objectives
Myocardial wall stretch is the main trigger for pro-brain natriuretic peptide (pro-BNP) secretion. The reduced heart rate associated with bradyarrhythmia increases stroke volume, resulting in increased wall tension. Therefore, we propose that bradyarrhythmia could increase plasma N-terminal pro-BNP (NT-pro-BNP) levels.
Subjects and Methods
We enrolled 125 patients who received a temporary pacemaker because they had sinus node dysfunction (SND) or atrioventricular blocks (AVBs). Patients with renal dysfunction, hyperkalemia, reduced left ventricular systolic function (left ventricular ejection fraction [LVEF], <40%), and atrial fibrillation were excluded. Heart failure (HF) was defined as an NT-pro-BNP level of >300 pg/mL. We evaluated history of hypertension, diabetes mellitus, and ischemic heart disease, plasma NT-pro-BNP levels, body mass index (BMI), LVEF, left atrial diameter (LAD), and escape rhythm rate.
Results
The log plasma NT-pro-BNP level of the patients with AVBs was significantly increased compared to that of the patients with SND (3.17±0.55 vs. 2.93±0.64 pg/mL, respectively; p=0.03). The incidence of HF was 72.5% (106 patients; 44 male patients). Further, the incidence of HF was significantly higher among patients with AVBs than among patients with SND. The type of bradyarrhythmia was found to be the only predictor of HF after adjusting for age, history of hypertension, LAD, and LVEF. The LVEF, LAD, and ventricular rate were similar between the 2 groups.
Conclusion
As in the case of patients with tachyarrhythmia, bradyarrhythmia may increase plasma NT-pro-BNP levels, leading to HF. Therefore, the possibility of HF should be considered in patients with bradyarrhythmia.
Introduction
Brain natriuretic peptide (BNP) and N-terminal pro-brain natriuretic peptide (NT-pro-BNP) have been used as markers for diagnosis or risk stratification in patients with heart failure (HF), stable coronary artery disease, and acute coronary syndrome [1]. BNP secretion is mainly triggered by myocardial wall stretch [2]. Tachycardia-induced cardiomyopathy is a well-known cause of arrhythmia-induced elevation in natriuretic peptide levels [3–5]. Therefore, we decided to investigate whether bradyarrhythmia causes an increase in plasma NT-pro-BNP levels.
Subjects and Methods
We retrospectively enrolled 125 patients who received a temporary pacemaker because they were found to have sinus node dysfunction (SND) or atrioventricular blocks (AVBs) at the emergency department of Daegu Catholic University Medical Center from March 2006 to February 2012. The SND cases included symptomatic marked sinus bradycardia (<40 bpm) or long sinus pause (>3.0 s). AVB cases included high degree AVBs or complete AVBs. Patients with renal dysfunction, hyperkalemia, reduced left ventricular systolic function (left ventricular ejection fraction [LVEF] <40%), and atrial fibrillation were excluded. Heart failure (HF) was defined as a NT-pro-BNP level of >300 pg/mL, as described in the 2012 European Society of Cardiology (ESC) Guidelines [6]. We evaluated history of hypertension, diabetes mellitus, ischemic heart disease, plasma NT-pro-BNP levels, body mass index (BMI), LVEF, left atrial diameter (LAD), and ventricular rate. Blood samples were drawn from patients within 1 hour after arrival at the emergency department, and specimens were placed in 5-mL ethylenediaminetetraacetic acid tubes and immediately centrifuged. Plasma NT-pro-BNP levels were measured by using an automated system (Elecsys 2010™, Roche Diagnostics, Indianapolis, IN, USA). The current study was conducted in accordance with the Declaration of Helsinki, and the Institutional Review Board of Daegu Catholic University Medical Center approved the study protocol.
Statistical analysis
The Statistical Package for the Social Sciences (SPSS) 19.0 (SPSS Inc., Armonk, NY, USA) statistical software package was used for all calculations. Data are presented as mean ± standard deviation for continuous variables and as percentages for categorical data. The included patients were divided into 2 groups (HF versus no HF) according to the measured plasma NT-pro-BNP levels. The unpaired Student t-test was used to analyze differences between each group. The categorical data were analyzed by using the chi-square test. The predictors of HF were analyzed by multivariate logistic regression. A p value of <0.05 was regarded as statistically significant.
Results
Baseline characteristics
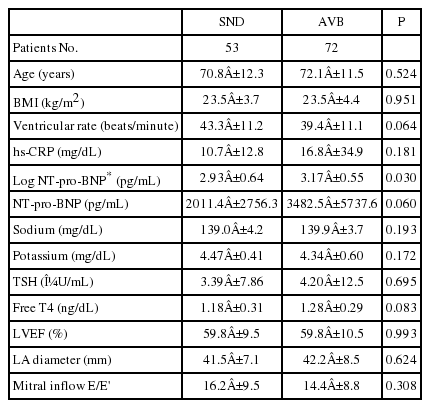
Table 1 shows the baseline characteristics of the patients with SND (n=53) and AVBs (n=72). Age and BMI did not differ between the 2 groups. In addition, the levels of electrolytes such as sodium and potassium, thyroid function, and transthoracic echocardiographic parameters such as LVEF, LAD, and mitral inflow pattern determined by using Doppler were similar between SND and AVB patients. The ventricular rate was found to be slower in patients with AVBs than in those with SND, although the difference was not significant. However, NT-pro-BNP levels were significantly higher in patients with AVBs than in those with SND (Figure 1).
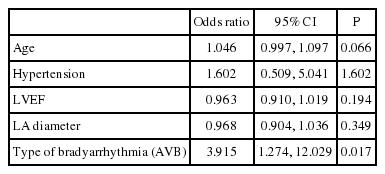
Differences in patient characteristics according to the incidence of HF
Table 2 shows the differences in patient characteristics according to the incidence of HF. A total of 166 patients (84.8%) were diagnosed with HF. The incidence of HF was significantly higher in patients with AVBs than in those with SND (66/72; 91.7% versus 40/53; 75.5%, respectively; p<0.05). The HF patients were significantly older and had lower BMI values than those without HF. Serum sodium levels were significantly lower in patients with HF as compared to those without HF. Transthoracic echocardiographic parameters were similar between the patients with and without HF. Multivariate analysis revealed that the presence of AVBs was the only independent predictor of HF after adjusting for age, history of hypertension, LVEF, and LAD (Table 3).
Discussion
The present study demonstrated that bradyarrhythmia can cause an increase in plasma NT-pro-BNP levels. Furthermore, NT-pro-BNP levels were higher in patients with AVBs as compared to those with SND.
Kovats et al. [7] reported that in elderly women with beta-blocker therapy-induced sinus arrest with a 40 bpm junctional escape rhythm and elevated NT-pro-BNP serum levels, the stroke volume increased at the lower heart rate in order to keep up the cardiac output. Increased stroke volume results in increased wall tension, which in turn triggers natriuretic peptide secretion [8]. Further, Meiracker et al. [9] demonstrated that in hypertensive patients, decreased heart rate due to beta-blocker therapy increased plasma atrial natriuretic peptide and BNP concentrations.
Pan et al. [10] reported that patients with SND, AVB, and atrial fibrillation had increased plasma NT-pro-BNP levels as compared to the controls, and NT-pro-BNP levels were lower in patients with SND than in patients with AVB; this finding is consistent with our result. They also demonstrated that the severity of atrioventricular asynchrony was an independent determinant of NT-pro-BNP levels. Atrioventricular asynchrony leads to stretching of the atrial wall and increased ventricular end-diastolic pressure, resulting in increased secretion of NT-pro-BNP from the atrium and ventricle [11–12]. Koch et al. [13] reported that patients with dual-chamber pacing had significantly lower BNP values as compared to those with single-chamber ventricular pacing due to the loss of atrioventricular synchrony.
Taken together, bradyarrhythmia due to beta-blocker therapy, AVBs, or SND can lead to elevated plasma NT-pro-BNP levels by increasing cardiac wall stretch through an increase in stroke volume or loss of atrioventricular synchrony (Figure 2).
Conclusion
As in the case of patients with tachyarrhythmia, bradyarrhythmia, especially that caused by AVBs, may cause an increase in plasma NT-pro-BNP levels, leading to HF. Therefore, the possibility of HF should be considered in patients with bradyarrhythmia.