|
|
International Journal of Arrhythmia 2012;13(3): 24-27.
|
Introduction
The duration of ventricular activation, or QRS
interval, is normally 60-100 ms. A widening of the QRS
interval indicates prolonged ventricular activation that
did not go through the normal conduction system.
Prolonged activation can be classified according to 3
groups with different root causes: (1) abnormal
conduction system (i.e., right or left bundle branch
block), (2) ventricular origin (i.e., VT/fibrillation), (3)
and ventricular preexcitation.
Most tachycardias are characterized by a wide QRS interval and are ventricular in origin, especially in
patients with structural heart disease. In cases of
patients with an abnormal conduction system,
including aberrancy or preexcitation, it is not easy to
differentiate VT from supraventricular tachycardia.
However, differential diagnosis is very important
because the treatments and prognoses differ
substantially.
In cases of VT, ventricular activation originates in
the ventricle itself and atrial activation originates in
the sinus node. Therefore, evidence of atrioventricular
dissociation is a strong indicator of VT. If, however,
either the typical morphology of a bundle branch block
or preexcitation is observed in the ECG, it would
suggest supraventricular tachycardia.
Case
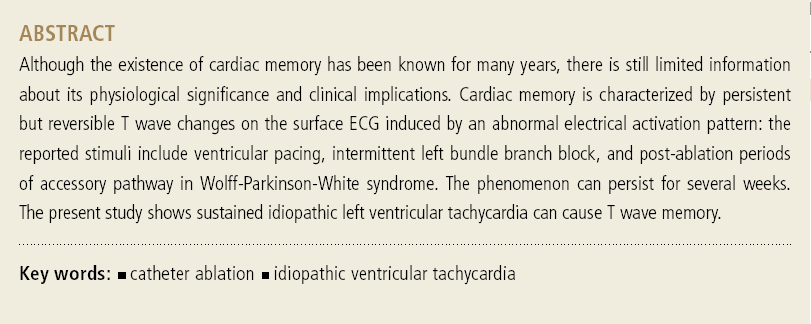
A 41-year-old man with a 3-hour history of
palpitations visited a local clinic and was referred to a
general hospital. His blood pressure was 100/70 mmHg
and his heart rate was 190 bpm. His ECG suggested
VT; therefore, the patient was administered amiodarone
infusion (300 mg loading dose and 900 mg/day
continuous infusion). The tachycardia persisted and
electrical cardioversion was attempted (biphasic 100 J,
200 J) but was unsuccessful. Verapamil injection also
failed to terminate the tachycardia. Therefore, the
patient was referred to our hospital. In the emergency
room, his heart rate decreased but the patient was still
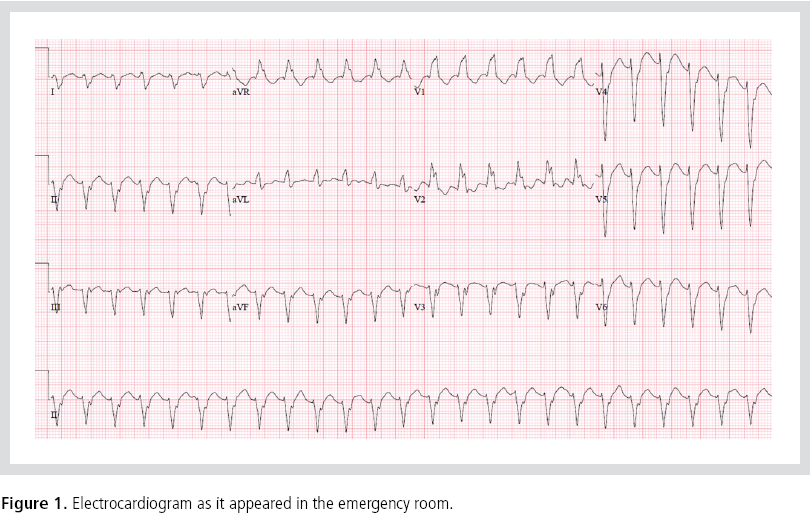
tachycardic (Figure 1). An electrophysiological study
was performed that immediately confirmed the
diagnosis of VT. A circuit was mapped in the area of the
posterior fascicle (Figure 2) and successfully terminated
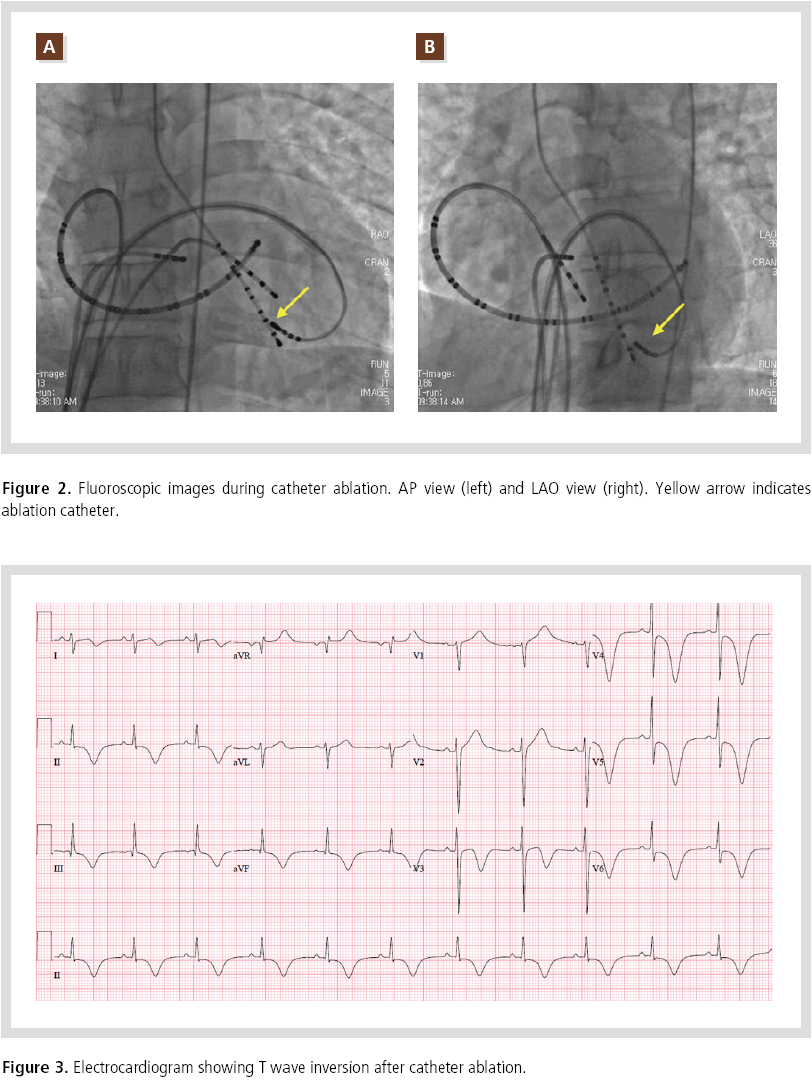
with ablation. After the procedure, surface ECGs
showed T wave inversion with the same vector as the QRS complex during VT (Figure 3). Serial cardiac
biomarker tests and echocardiograms showed no
evidence of myocardial infarction or ischemia. The
occurrence of T wave memory caused by prolonged VT
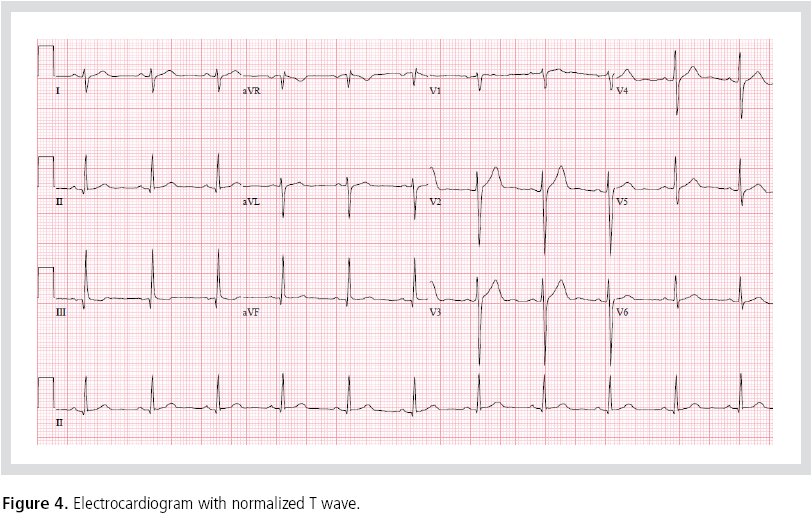
was hypothesized. One month later, the T wave
inversion had disappeared (Figure 4). The patient was
followed for 6 months. Antiarrhythmic medication was
not prescribed and there was no recurrence during this
time.
Discussion
Of the 3 waveforms in the ECG: the P wave reflects
atrial activation, the QRS complex is associated with
ventricular activation, and the T wave indicates
ventricular repolarization. Cardiac memory is most
clearly seen in the T wave. T wave changes occur in
various circumstances and are referred to as primary
or secondary.1 Primary T wave changes are derived
entirely from the ion channel and electrical determinants of repolarization, and are independent of
the QRS complex;2 for instance, the changes occurring in patients with hyperkalemia or hypokalemia.
Secondary T wave changes, on the other hand, arise from an altered sequence of activation and are
dependent on the QRS complex. Such T waves can be
observed during ventricular pacing or ventricular
arrhythmia, and may occur in normal or diseased
hearts. After a period of abnormal activation (i.e.,
ventricular pacing, sustained ventricular arrhythmia,
or preexcitation), a change in the T wave can persist
even after sinus rhythm and normal activation are
returned. In these cases, the T wave retains the vector
of the previously abnormal QRS complex.3 Long
periods of abnormal activation can increase the
magnitude of these T wave changes; this is referred to
as accumulation. The duration of T wave memory can extend far beyond the termination of the inciting
stimulus, persisting even after normal rhythm and
activation return.
References
- Katz AM. T wave “memory”: possible causal relationship to
stressinduced changes in cardiac ion channels?
J Cardiovasc
Electrophysiol.
1992;3:150-159.
- Rosen MR. The heart remembers: clinical implications.
Lancet.
2001;357:468-471.
- Shvilkin A, Danilo P Jr, Wang J, Burkhoff D, Anyukhovsky EP,
Sosunov EA, Hara M, Rosen MR. Evolution and resolution of
long-term cardiac memory.
Circulation.
1998;97:1810-1817.
|
|
|
|